Case Report - (2023) Volume 8, Issue 4
Usefulness Of The Toric Alignment Check Module Of The Itrace Analyser In Assessing The Alignment Of An Intraocular Toric Lens In Relation To The Axis Of Corrected Corneal Astigmatism Postoperatively
Received Date: Mar 23, 2023 / Accepted Date: Apr 12, 2023 / Published Date: Apr 20, 2023
Abstract
Correct alignment of an intraocular toric lens in relation to the axis of corneal astigmatism is, next to the precise calculation of its value, the most important element that allows for the best possible postoperative vision to be obtained. However, it is not always possible to achieve this during lens implantation. In the era of an increased number of implantations of multifocal, complex intraocular lenses, it is sometimes unknown whether the reason for poor visual acuity lies in the complexity of the lens structure or in its misalignment in relation to the axis of corneal astigmatism. In such cases, programs indicating whether the lens has been aligned with the axis of corneal astigmatism are helpful. The “Toric Alignment Check” module of the iTrace analyser is one of them. The study describes thirteen cases of axial misalignment of toric lenses and the change in the quality of vision and visual acuity after its rotation to the correct axis using the above module.
Keywords
Intraocular Toric Lens, Toric Alignment Check, Corneal Astigmatism.
Introduction
Corneal astigmatism is an element of the optical system of the eye that requires taking the postoperative aphakia into account in the correction process. According to many authors, corneal astigmatism values above 0.75Dcyl should be corrected with toric intraocular lenses in the case of lens removal. Is this true? Considering the fact that the posterior surface of the cornea can correct up to 0.75 dioptres of astigmatism generated by the anterior surface of the cornea, it seems that the subject is more complex. Here, it is worth adding that only regular corneal astigmatism is subject to correction. Proper correction of astigmatism is of particular importance in young people with diagnosed presbyopia, who, wanting to get rid of their refractive error, have been recommended implantation of a complex multifocal lens. Lack of proper correction of astigmatism impairs vision in terms of quality and visual acuity.
Byeong-Yeon Moon et al. described how uncorrected astigmatism reduces visual acuity. Uncorrected astigmatism at the level of 4 dioptres means loss of vision at the level of 90%. Below, the correlations between the obtained visual acuity to far distances (decimal chart) and the value of uncorrected astigmatism (dioptres) are indicated: 1.0/0.25 D, 0.9/0.50 D, 0.8/0.75 D, 0.7/1.00 D, 0.6/1.25 D, 0.5/1.50 D, 0.4/2.00 D, 0.3/2.50 D, 0.2/3.00 D, 0.1/4.00 D, and 0.05/4.75 D [1].
While Wolffsohn et al. point out that uncorrected astigmatism impairs not only vision to far and near distances, but also its quality [2]. One of numerous examples (the case presented by the author) shows the huge significance of correction of astigmatism.
Male, age 45, diagnosis: presbyopia, preoperative hyperopia +2.0Dsph. The patient wishes to get rid of his refractive error. Preoperative best-corrected visual acuity to far distances (BCVA) is 0.0 logMar. Preoperative keratometry and corneal topography showed regular astigmatism of 1.25Dcyl, but refractometry showed only astigmatism of +0.5Dcyl. His astigmatism has never been corrected because it was not needed. In the process of refractive lens exchange (RLE), the patient was implanted a trifocal spherical lens. One month after surgery, best, uncorrected visual acuity (UCVA) to far distances was 0.2 log Mar, which was 2 lines worse as compared with BCVA before surgery. The patient additionally complained that his vision was blurred. The eye examination showed that astigmatism correction at the level of 0.5-0.75Dcyl improves vision. Due to the presence of a refractive error in keratometry with a value of +1.25Dcyl, a decision was made to perform a limbal relaxing incision (LRI), after which astigmatism decreased to 0.5Dcyl. BCVA reached 0.0 logMar and quality of vision improved.
The decrease in visual acuity in the absence of correction of astigmatism applies to phakic and pseudophakic eyes. Hoshikawa et al. showed a correlation between the value of astigmatism and the probable loss of visual acuity to far distances, assessed in a group of 318 patients, of whom 160 were pseudophakic [3]. The obtained values are presented below in Table 1.
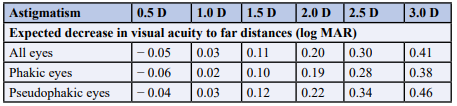
Table 1: Correlation between the value of uncorrected astigmatism and the predicted decrease in visual acuity in eyes with natural lens and pseudophakic eyes. The greater the value of uncorrected astigmatism, the greater the loss in visual acuity
Does it make sense to correct corneal astigmatism below 0.5Dcyl? Villegas et al. believe that such an astigmatism value does not cause a decrease in visual acuity. The authors add, however, that correction of astigmatism had a positive effect on the quality of vision [4]. For many patients, this is of great importance. Taking into account our own observations, correction of such mild astigmatism should always be taken into account, especially in the case of implantation of complex lenses in young people. In people with a wide pupil, especially in scotopic conditions, correction of mild astigmatism becomes of great importance.
When deciding to correct astigmatism with the use of a toric lens, there are several pitfalls waiting for the physician, and therefore also for the patient. One of them is the alignment of a toric lens. There are certain well-established rules as to the position of the patient’s body in which the axis of astigmatism should be determined. The axis should never be determined with a patient in the supine position due to the possible cyclorotation of the eyeball. The physician can choose from many programs that allow to determine preoperatively and indicate intraoperatively the correct axis of corneal astigmatism. Unfortunately, there are situations when after the implantation of a toric lens, visual acuity to far distances does not reach its full value and vision is blurred.
In the case of monofocal toric lens implantation, refractometry and diagnosis of astigmatism of the entire optical system, the axis of which is different from the corneal astigmatism axis, gives us information about the high probability of non-axial implantation of the toric lens (Figure 1).
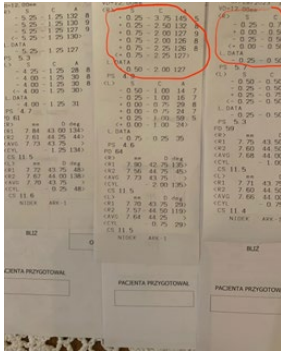
Figure 1: Refractometry performed: before the procedure (left side), one month after implantation of a toric lens, values from the right eye circled in red (middle result)-the presence of astigmatism, despite its correction, draws attention. Result-right side, condition after correcting the lens alignment to the correct axis of the cornea, disappearance of astigmatism is noticeable.
In general, when a monofocal toric lens is properly calculated and properly aligned in relation to the corneal astigmatism axis, refractometry should show a very low astigmatism value of no more than 0.75 Dcyl. However, the value of residual astigmatism should be smaller in the case of implantation of custom toric lenses, assuming that it has been properly calculated.
The situation is more complicated when a toric, multifocal lens is implanted. Why? The author’s own research, described in the article “Assessment of the Value of Astigmatism Generated by Two Models of Spherical Multifocal Lenses: Panoptix® by Alcon® and Acunex Variomax® by Teleon® using the Toric Alignment Check Module of the Itrace Analyser” showed that multifocal lenses with a spherical structure “generate” artificial astigmatism, which is visible, among others, in refractometry and in the examination using the iTrace analyser [5].
Below are two examples of results obtained using the “Toric Alignment Check” module, performed postoperatively after implantation of spherical lenses, one with a bifocal, asymmetric structure, the other with a diffractive structure. The results clearly indicate internal astigmatism generated by these lenses (Figure 2a,b). If we focused more on the presence of astigmatism in postoperative refractometry, we could say that it appears in many cases after the implantation of lenses with a spherical structure.
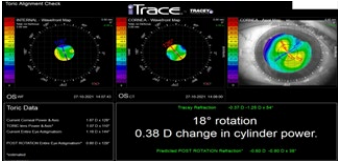
Figure 2a: The result of the examination performed using the “Toric Alignment Check” module, in the eye with the implanted spherical lens with a bifocal asymmetric structure.
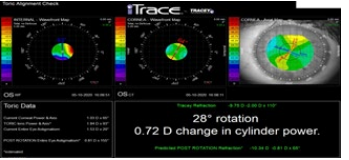
Figure 2b: After implantation of a spherical lens with a trifocal diffraction structure. In both cases, the results suggest the presence of internal astigmatism, generated by lenses with a spherical structure.
In view of the above, in the case of blurred postoperative vision and the implantation of complex toric lenses, more inquisitive doctors have doubts whether it is caused by its axial misalignment or the complexity of the lens structure. Misalignment of a toric lens requires correction of its position. Misalignment of the lens means the already mentioned loss of visual acuity and quality of vision. Misaligning the toric lens in the wrong axis, exceeding the value of 30 degrees results in almost complete loss of its corrective properties in terms of astigmatism [6].
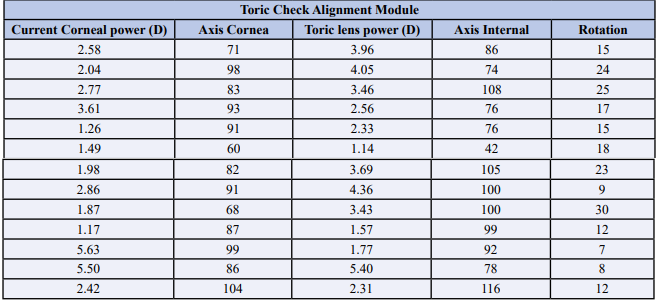
In the case of correction of large astigmatism values, rotating the axis by several degrees can cause a significant decrease in visual quality and visual acuity (author’s note). In the everyday practice of the author of the article, the tool that allows to solve this problem is the iTrace® analyser, and more precisely the “Toric Alignment Check” module. A typical test result using this module is presented in Figure 3.
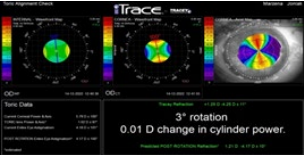
Figure 3: A sample result of the examination performed using the “Toric Alignment Check” module of the iTrace analyser.
Top three blocks: Top-left: toric intraocular lens alignment axis, top-centre: corneal astigmatism axis, top-right: result of corneal topography. Bottom blocks: bottom-left: “Toric Data”, information on corneal astigmatism value and axis, residual astigmatism value and axis (TORIC Lens Power and Axis®), and current entire eye astigmatism generated by the toric lens. The last item in this block is the estimated value of post-rotation entire eye astigmatism. Bottom-right: information about by how many degrees and in what direction the lens should be rotated, and by what cylindrical value astigmatism will decrease after its rotation. The value of this information is enormous. When deciding to rotate the toric lens to the correct corneal axis, the examination using the “Toric Alignment Check” module significantly facilitates this.
As already mentioned, corneal astigmatism above 0.75Dcyl requires correction. In a situation where a 60-year-old patient with diagnosed cataract and corneal astigmatism at the level of 1.0 Dcyl that has never been corrected will not notice a major difference in vision if astigmatism is not corrected during surgery, a young 40-year-old person with the same astigmatism, in the case of whom the contrast of vision is much better in the absence of correction of astigmatism will certainly experience a deterioration of vision after the procedure.
Objective of the Study
Evaluation of the usefulness of the examination using the iTrace analyser with the “Toric Alignment Check” module in the assessment of postoperative alignment of a toric intraocular lens in relation to the axis of corneal astigmatism.
This device combines the functions of an aberrometer and a corneal topographer. Thanks to this combination, iTrace has many diagnostic advantages, and the “Toric Alignment Check” module allows for the assessment of the alignment of a toric intraocular lens in relation to the axis of corneal astigmatism.
Eleven patients, thirteen eyes with corneal astigmatism requiring correction, were included in the study. Four patients (6 eyes) underwent cataract surgery, and the remaining patients underwent refractive lens exchange (RLE). In two patients (4 eyes) a monofocal toric lens was implanted; in the remaining patients implantation involved multifocal toric lenses, including bifocal (3 eyes), trifocal (1 eye), 5 focal (1 eye), EDOF (3 eyes) and complex, including a combination of EDOF with a trifocal structure (1 eye). Toric Alignment Check was performed for two main reasons. The first reason is inadequately poor, postoperative visual acuity to far distances, much worse than expected. The second reason is the presence of astigmatism in refractometry, the value of which was too high in relation to the predicted one and its axis differed from the axis of corneal astigmatism.
Examination Technique
The examination using the iTrace analyser was performed one month after lens removal, and was preceded by a full eye examination, assessing whether and how correction of the detected astigmatism affects vision. The examination using the “Toric Alignment Check” module was performed in scotopic conditions, without prior pupil dilation. The examination was repeated three times at short intervals. Patients who obtained reproducible results with the misalignment of a toric lens with respect to the axis of corneal astigmatism were qualified for the lens rotation procedure (Figure 4).
Figure 4: Results of the examination performed using the “Toric Alignment Check” module in a 47-year-old patient, after RLE with implantation of a toric lens with an EDOF structure. BCVA to far distances before surgery=0.1 log Mar, after surgery UCVA=0.2 log Mar, which is worse than the preoperative value.
The lens was rotated by about 14°, obtaining a value of 0.1. In the case of this patient, the presence of a spherical defect, which could be corrected by, among others, implanting an additional spherical lens, additionally draws attention.
Procedure Technique
Having obtained the result of the examination using the “Toric Alignment Check” module, two matters were established:
1. By how many degrees should the lens be rotated
2. In which direction to rotate the lens to align it with the axis of corneal astigmatism.
After separating the intraocular lens from the capsule using a viscoelastic, the lens was rotated by the value in degrees shown by the iTrace result. This value was determined in a simple way, thanks to the so-called Tocular, i.e. an eyepiece with an axial scale, mounted to one of the ophthalmic microscopes (Figure 5). In the case of lenses with 4 haptics, rotation could be performed safely in both directions, and in the case of lenses with two haptics, rotation to the correct axis was always performed clockwise.
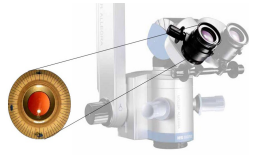
Figure 5: It presents an eyepiece with a scale, mounted to a microscope, facilitating the determination of the axis in the cornea. It is helpful, among others, in the case of toric lens implantation and determining the ranges of limbal relaxing incisions.
Results
The range of the corrected preoperative spherical error ranged between high myopia -24.5D and high hyperopia +8.0Dsph. Corrected corneal astigmatism showed values ranging from 1.5 to 5.75 Dcyl. Toric Alignment Check showed misalignment of the toric lens in relation to the axis of the corneal astigmatism. The examination results obtained using the above module are presented in Table 2.
The average rotation value was 16.5°, ranging from 7° to 30°. Lens rotation was performed in each case. After lens rotation, mainly two parameters changed, i.e. visual uncorrected acuity to far distances (UCVA) and the quality of vision to far and near distances. Visual acuity to near distances did not change significantly. Mean values of visual acuity to far and near distances, before and after rotation, are presented in Table 3 below.

Improvement in visual acuity was achieved in all cases, although in one patient (1 eye) the improvement in visual acuity did not improve the quality of vision. It is difficult to get statistics on such a small group of patients, but the correlation between a large loss of visual acuity in eyes where high astigmatism was corrected and even small lens misalignment, as well as the correlation between a low value of corrected astigmatism and a high value of lens misalignment draw attention. If you add to this the complexity of the lens structure, the effect of impaired vision is noticeable to a greater extent. Below are three examples of misalignment of the toric lens with a different structure, in eyes with various preoperative refractive error.
Case 1
Misalignment of a complex toric lens (trifocal + EDOF) in a patient with cataract and preoperative myopic astigmatism.
Male, 56, preoperative refractometry -3.25Dsph/-2.5Dcyl. BCVA to far distances (logMar), before surgery=0.3, after surgery UCVA = 0.2. Postoperative refractometry showed the presence of an error=-0.25 Dsph/-1.5Dcyl, the correction only slightly improved vision, therefore Toric Alignment Check was performed. The result indicated misalignment of the lens and the need for its rotation by 12 degrees. Rotation was performed clockwise. Improvement in the quality of vision and visual acuity to far distances was obtained, to the value of 0.0 logMar. UCVA to near distances remained unchanged obtaining the value of D-0.5 (Snellen). Post-rotation refractometry=0.25Dsph/- 0.25Dcyl (Figure 6a, b).
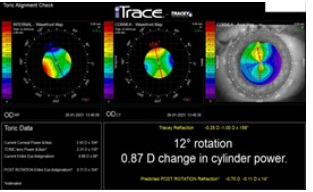
Figure 6 a: The result of the examination performed using the “Toric Alignment Check” module showed axial lens misalignment. The lens alignment axis is 116° and the corneal astigmatism axis is 104°, so the procedure will involve a 12° rotation
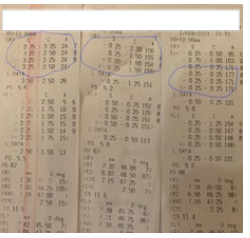
Figure 6 b: Three refractometry results taken in the eye after implantation of a toric lens. The result taken before surgery (left), after surgery (middle) and after lens rotation (right). The values obtained from the right eye are circled.
Case 2
Misalignment of a custom toric lens with a bifocal structure, asymmetric in both eyes with high myopia. Patient, 53 years old. Preoperative refractometry showed an error of -24.74 Dsph/-4 Dcyl in the right eye, and an error in the left eye, as well as corneal astigmatism of both eyes at 3.75Dcyl. Postoperative UCVA to far distances: right eye=0.4, left eye=0.3 logMar, to near distances in both eyes=D-0.5 (Snellen). The patient was very satisfied with the obtained result, mainly with the quality of vision. Due to the fact that in the right eye postoperative visual acuity to far distances was 1 line worse than preoperatively, Toric Alignment Check was performed. Examinations showed lens misalignment in both eyes, requiring rotation, in the right eye by 8° and in the left eye by 9° (Figure 7a, b). Rotation was performed in both eyes. Visual acuity to far distances improved in both eyes, reaching amazing values for the patient, i.e. 0.0 in the right eye and 0.1 logMar in the left eye. Vision to near distances did not change. What is very important is that refractometry after the procedure showed the presence of an “artificial” error in both eyes (right eye -1.0Dsph/-1.25Dcyl, left eye -1.5Dsph/-1.5Dcyl). It results from the lens structure.
It is worth emphasizing here that in the case of implanting a complex lens, regardless of whether it has a spherical or toric structure, before the patient is recommended to have their error found in refractometry corrected, an eye examination should be performed to assess the legitimacy of the procedure. In most cases, despite the error found in refractometry, no correction is required due to full visual acuity.
Case 3
Misalignment of a custom monofocal toric lens in eyes with high hyperopia. Patient, 70 years old, hyperopia in both eyes, diagnosed with immature cataract, corneal astigmatism, anisometropia and amblyopia of the right eye. Preoperative error and BCVA to far distances (logMar): right eye +8.0Dsph/- 3.0Dcyl=0.4, left eye +5.75Dsph/-2.75Dcyl =0.3, to near distances in both eyes, corrected=D-0.5. Implantation of a custom monofocal toric lens was performed in both eyes. Due to the worse value of postoperative visual acuity to far distances in the right eye (0.5 logMar) compared to vision before the procedure and the presence of a residual error in both eyes, Toric Alignment Check was performed. The examination showed lens misalignment (Figure 7).
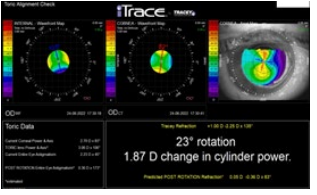
Figure 7: The result of the examination performed using the “Toric Alignment Check” module in the right eye after implantation of a toric monofocal custom lens. Its axial misalignment was demonstrated, requiring a rotation of 23°.
The lens rotation procedure was performed as indicated, in the right eye by 23°, in the left eye by 30°. Refractometry showed regression of the error and improvement of UCVA to far distances (right eye 0.3, left eye 0.1 LogMar). Refractometry showed: right eye, before rotation +2.0Dsph/-1.75Dcyl, after rotation +1.0Dsph/-0.25Dcyl, left eye: before rotation +1.5Dsph/- 2.25Dcyl, after rotation 0.0Dsph/-1.0Dcyl. In the case of a patient with several causes of poor postoperative visual acuity, including complexity of the lens structure or lens misalignment, lens misalignment must be checked.
Discussion
As already mentioned, in the case of implantation of a monofocal toric lens, its misalignment is quite easy to determine. This is due to the difference between the axis and astigmatism shown in refractometry and the axis of corneal astigmatism shown in keratometry or corneal topography. This condition additionally affects visual acuity and quality of vision.
The situation becomes more complex when a toric multifocal lens is implanted. Then, determining whether the cause of poorer visual acuity results from its misalignment or the complexity of the lens structure is difficult to determine only by comparing the axis of astigmatism and the axis of the cornea. Why? The very complexity of the lens structure affects the result of refractometry. Even spherical lenses can cause astigmatism in refractometry [5]. In such situations, lens alignment relative to the corneal axis should be assessed, and only at a later stage should other causes of poorer visual acuity be sought.
When analysing the above results of misalignment of a toric lens, it is necessary to find its causes. First of all, the correct axis of corneal astigmatism should be established. If the result of corneal topography repeated several times, shows the same values, determination of the axis can be considered appropriate. This result can be compared with the values obtained in keratometry in refractometry and during the calculation of the intraocular lens.
Unfortunately, these results may differ significantly in the case of calculating the lens in the eye with a significant decrease in visual acuity, e.g. due to mature cataract. Then, the patient does not cooperate as expected. Without knowing the patient, it is sometimes difficult to determine whether mild astigmatism that requires correction (e.g. 1.5 Dcyl) is real or results from the position of the eyeball. In such a situation, the history of correction of the patient’s error can help. However, if astigmatism has never been corrected before, it is better to implant a spherical lens into the eye and correct astigmatism postoperatively with a corneal relaxing incision or laser correction of the refractive error. There are many more reasons that may negatively affect the determination of the correct axis of astigmatism. It is worth mentioning refractive errors, large alpha angles, strabismus, conditions after eye injury or macular degeneration.
Assuming that the toric lens has been properly calculated, there is one more important step in the treatment, i.e. lens alignment in the eye. The already mentioned correct position of the patient during the determination of the axis is of great importance. There are numerous programs available on the market allowing for the determination of the correct axis intraoperatively with high precision, but we can never be sure whether the lens has been aligned in the eye in the right axis. In the case of inadequately poorer postoperative visual acuity and quality of vision, it is worth checking the alignment of the toric lens.
Conclusion
The examination performed using the iTrace analyser, the “Toric Check Alignment” module, precisely showed the misalignment of the toric lens in relation to the corneal axis in the group of patients in whom such a suspicion existed due to reduced visual acuity. Due to the obtained results, the lens was rotated in each case by the value shown in the examination. In each case, the quality of vision and visual acuity improved.
References
1. Moon, B., Kim, S., & Cho, H.G. (2013). Predicting of Uncorrected Astigmatism from Decimal Visual Acuity in Spherical Equivalent. Journal of The Optical Society of Korea, 17, 219-223.
2. Hoshikawa, R., Kamiya, K., Fujimura, F., & Shoji, N. (2021). Prediction of distance visual acuity in presbyopic astigmatic subjects. Scientific reports, 11(1), 6958.
3. Villegas, E. A., Alcón, E., & Artal, P. (2014). Minimum amount of astigmatism that should be corrected. Journal of cataract and refractive surgery, 40(1), 13-19.
4. Wolffsohn, J. S., Bhogal, G., & Shah, S. (2011). Effect of uncorrected astigmatism on vision. Journal of cataract and refractive surgery, 37(3), 454-460.
5. Cywinski, A., Bloch, D., &Lubczyk, A. (2022). Assessment of the Value of Astigmatism Generated by Two Models of Spherical Multifocal Lenses: Panoptix® by Alcon® and Acunex Variomax® by Teleon® using the Toric Alignment Check Module of the Itrace Analyser. Open Access Journal of Ophthalmology, 7(2), 2022.
6. Christopher, K (2017) Toric IOLs: Nailing the Target Meridian. Review of Ophthalmology, 2017
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



