Research Article - (2025) Volume 10, Issue 1
Systematic Review and Meta-Analysis of Traditional Chinese Medicine Bath in the Treatment of Neonatal Jaundice
2Department of Obstetrics, The First Affiliated Hospital of Guizhou University of Traditional Chinese, China
3Department of Pediatrics, The First Affiliated Hospital of Guizhou University of Traditional Chinese, China
Received Date: Dec 31, 2024 / Accepted Date: Jan 06, 2025 / Published Date: Jan 25, 2025
Copyright: Copyright: ©2025 Wei Sun, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited.
Citation: Sun, W, Zhao, X, Wu, Z., Yu, H., Wang, Y, et al. (2025). Systematic Review and Meta-Analysis of Traditional Chinese Medicine Bath in the Treatment of Neonatal Jaundice. J Clin Rev Case Rep, 10(1), 01-10.
Abstract
Using meta-analysis method, evaluate the clinical efficacy and safety of traditional Chinese medicine bath in the treatment of neonatal hyperbilirubinemia, and use data mining techniques related to the "Ancient and Modern Medical Case Cloud Platform (V2.3.4)" to study the medication rules of the involved traditional Chinese medicine formulas, providing evidence-based medicine for the clinical application of traditional Chinese medicine bath in the treatment of neonatal hyperbilirubinemia. Search the Chinese Biomedical Literature Database (SinoMed), Chinese Academic Journal Online Publishing Database (CNKI), Wanfang full-text database, Chongqing VIP Chinese Science and Technology Journal Database, Cochrane Library, Embase, PubMed, and manually search for randomized controlled clinical trials related to traditional Chinese medicine bath treatment for neonatal hyperbilirubinemia in conference papers, with a time limit from the date of establishment to October 2024.
Two trained researchers independently screened literature and collected research data based on inclusion and exclusion criteria. They used the bias risk assessment tool provided by the Cochrane Collaboration and RevMan 5.3 software to evaluate the quality of the included literature and conduct meta-analysis. The traditional Chinese medicine formulas involved in the included literature were entered into the "Ancient and Modern Medical Case Cloud Platform (V2.3.4)" to explore the medication rules of traditional Chinese medicine bath treatment for neonatal hyperbilirubinemia.
Meta-Analysis: A total of 34 randomized controlled trials (RCTs) were obtained on the treatment of neonatal hyperbilirubinemia with traditional Chinese medicine baths, involving 7965 patients. Among them, 4021 patients were in the experimental group and 3944 patients were in the control group. The total effective rate of traditional Chinese medicine bath combined with conventional treatment in the treatment of neonatal hyperbilirubinemia is better than that of conventional treatment alone; Compared with conventional treatment alone, the combination of traditional Chinese medicine bath and conventional treatment can reduce the total bilirubin level and shorten the treatment time in the treatment of neonatal hyperbilirubinemia. In the treatment of neonatal hyperbilirubinemia, the traditional Chinese medicine formulas often contain drugs with bitter and cold flavors. The method is to clear heat and dampness, promote bile flow and eliminate jaundice. While clearing liver and gallbladder dampness and heat, the spleen and stomach are also taken into account.
The use of bitter and cold drugs is effective in regulating the pathogenic factors of dampness and heat. The medication reflects the use of the method of inhibiting wood and supporting soil to regulate the liver and spleen, and according to the changes in the disease, combined with the symptoms of the child, it is treated accordingly.
Keywords
Neonatal hyperbilirubinemia, Traditional Chinese Medicine Bath, Meta-analysis, Medication rules
Introduction
Neonatal hyperbilirubinemia is one of the most common diseases in newborns, characterized by excessive bilirubin production, abnormal bilirubin excretion, and increased enterohepatic circulation. It is caused by abnormal elevation of bilirubin in the blood of infants, resulting in skin and sclera jaundice as the main manifestations. About 50% of full-term infants and 80% of premature infants will experience visible jaundice. Because most newborns may experience skin and sclera jaundice during normal growth and development, and some diseases may also present with skin and sclera jaundice, some families of the affected children overlook the harm of neonatal hyperbilirubinemia. Among them, 0.9% of the affected children may develop bilirubin encephalopathy, leaving neurological sequelae that prevent them from taking care of themselves in their future life and studies, causing a certain burden on society and families. Studies have shown that neonatal hyperbilirubinemia may be associated with autism and may increase the risk of developing autism in children [3-5]. Therefore, early and accurate identification of neonatal hyperbilirubinemia and timely, safe, and effective intervention are key to preventing severe hyperbilirubinemia and bilirubin encephalopathy, which is of great significance for the healthy growth of children. At present, in addition to Western medicine treatment methods such as phototherapy, drug therapy, and exchange transfusion therapy, traditional Chinese medicine treatment also plays an important role. Among them, phototherapy is a common method for neonatal hyperbilirubinemia. The treatment principle is that lipophilic bilirubin is oxidized and hydrolyzed into water-soluble isomers under blue-green light irradiation of a certain wavelength, and is directly excreted from the body through bile, feces, and urine; Adverse reactions of phototherapy occur from time to time, such as diarrhea, erythema, fever, dehydration, rash, etc. in children. Drug therapy, including liver enzyme inducers, intestinal probiotics, zinc supplements, intravenous immunoglobulin and albumin, can increase the financial burden on the child's family, and its adverse reactions such as allergies, drowsiness, and poor response can affect the child's recovery. For severe hyperbilirubinemia, blood exchange therapy is necessary. Although the efficacy is certain, complications such as electrolyte imbalance, circulatory overload, coagulation dysfunction, arrhythmia, etc. cannot be ignored, and there is even a risk of death.
Traditional Chinese Medicine classifies neonatal hyperbilirubinemia as "fetal jaundice" or "fetal jaundice". The disease name, etiology, and pathogenesis were first discussed in the book "Treatise on the Origin and Symptoms of Various Diseases. Fetal Gallbladder Symptoms" written by Chao Yuanfang in the Sui Dynasty. The book states: "When a child is in the fetus, the mother's internal organs and qi are hot and fumigated in the fetus, causing the entire body of the child to be yellow, which is called fetal jaundice. Iron Mirror for Preschool Science, etc. Traditional Chinese medicine has a long history of understanding and treating fetal jaundice and jaundice, and Western medicine treatment plans have many limitations and shortcomings mentioned above, which has led to more and more clinical doctors using traditional Chinese medicine to treat this disease. The number of published clinical research literature is also increasing, accumulating a lot of clinical experience, indicating that the advantages of traditional Chinese Medicine in treating neonatal hyperbilirubinemia have been recognized by a large number of clinical doctors. The treatment of neonatal hyperbilirubinemia with traditional Chinese medicine mainly relies on traditional Chinese medicine baths, which have the characteristics of simplicity, convenience, affordability, and practicality, and are easily accepted by children and parents. However, many clinical studies and reports on the use of traditional Chinese medicine baths to treat neonatal hyperbilirubinemia lack standardization. On the other hand, due to the fact that research on the treatment of neonatal hyperbilirubinemia with traditional Chinese medicine baths mainly focuses on control observation and case reports, the authenticity and reliability of the research results are questioned.
Therefore, this study will adopt the internationally recognized scientific research method of meta-analysis, which can provide high-quality evidence-based medicine evidence. Meta-analysis can solve the problems of bias and inaccurate statistical results caused by small sample size, and systematically evaluate the efficacy and safety of randomized controlled clinical trials of traditional Chinese medicine bath treatment for neonatal hyperbilirubinemia, in order to provide high-quality evidence-based medicine support for the clinical use of traditional Chinese medicine bath treatment for neonatal hyperbilirubinemia. At present, there is no unified or widely recognized traditional Chinese medicine anti yellowing external cleansing agent in clinical practice. Most of them are self-formulated formulas or hospital preparations based on classic ancient Chinese medicine formulas, and clinical doctors have flexible and varied approaches to medication. Different doctors have different understandings of diseases and drugs, making it difficult to grasp the medication rules.
However, domestic researchers have used the data mining technology of the "Ancient and Modern Medical Case Cloud Platform" system to study the medication rules of database journal literature, famous traditional Chinese medicine practitioners' experiences, and medical cases [7-9]. Therefore, the traditional Chinese medicine formulas involved in previous system evaluations were entered into the "Ancient and Modern Medical Case Cloud Platform (V2.3.4)" for data mining to further explore their medication rules and contribute to the inheritance of traditional Chinese medicine. Provide evidence-based support for development.
Materials and Methods
Inclusion Criteria
Research subjects: Children diagnosed with neonatal hyperbilirubinemia with clear Western or Traditional Chinese Medicine diagnostic criteria. Traditional Chinese medicine syndrome classification, gender, region, and race are not limited.
Intervention measures: Children in the treatment group were given traditional Chinese medicine baths or traditional Chinese medicine baths on the basis of treatment in the control group. Not considering details such as treatment duration, bathing time, medication dosage, etc.
Control measures: Children in the control group were given routine treatment (including blue light irradiation, traditional Chinese patent medicines and simple preparations, liver enzyme inducer, nutritional support, intestinal probiotics, antibiotics, albumin, etc.).
Outcome measures: Main outcome measures: Total effective rate and total bilirubin level after treatment; Secondary outcome measures: length of hospital stay, duration of jaundice, duration of phototherapy, and adverse reactions.
Research type: Inclusion in publicly published randomized controlled clinical trials, regardless of whether allocation concealment schemes and blinding methods are described, published in both Chinese and English.
Literature Research
Retrieve randomized controlled clinical trials on traditional Chinese medicine bath therapy for neonatal hyperbilirubinemia from the Chinese Biomedical Literature Database (SinoMed), Chinese Academic Journal Network Publishing Database (CNKI), Wanfang full-text database, Chongqing VIP Chinese Science and Technology Journal Database, Medline, the Cochrane Library, and PubMed through computer search. The time limit is from the date of library establishment to October 2023. In addition, manually search for literature related to neonatology and pediatrics conferences to screen for clinical studies that meet the inclusion criteria.
The key words for the title of the article in Chinese are neonatal hyperbilirubinemia, erythropoiesis, neonatal jaundice, fetal jaundice, neonatal pathological jaundice, traditional Chinese medicine bath, traditional Chinese medicine external washing, traditional Chinese medicine fumigation washing, and traditional Chinese medicine soaking bath; The key words for the title of the article in English are Neonatural jade, Neonatural hyperbilirubinemia, Hydrotherapy baths, Chinese Herbal drug, and Chinese Traditional Medicine.
Literature Screening Management and Data Extraction
Each literature is individually screened by two researchers to determine its inclusion. If there is any disagreement, both parties will discuss and resolve it, and if necessary, a third party will arbitrate. After importing the search literature, the selection of literature materials is divided into three steps: â? plagiarism check: first screen out all duplicate literature; â?¡ Initial screening: Screen out unqualified literature based on the title and abstract of the article; â?¢ Re screening: Read and analyze the remaining literature one by one to determine whether they are included. The quality analysis of research methods is conducted according to the four criteria for randomized controlled trials in the literature [10].
Statistical analysis
Using Review Manager 5.3 software. For binary variables with unified measurement units, the risk ratio (RR) is used, and for continuous variables, the mean differences (MD) are used as the statistical measure for efficacy analysis. The estimation of each effect size interval is represented by a 95% confidence interval (CI). The heterogeneity test of each experimental result is conducted using chi square test. If there is no statistical heterogeneity (P>0.10, I2≤50%), a fixed effects model is selected for meta-analysis; If there is heterogeneity in the included studies, analyze the sources of heterogeneity and conduct a five group analysis of factors that may lead to heterogeneity; If there is statistical heterogeneity among studies but no clinical heterogeneity, a random effects model is chosen. P<0.05 is considered statistically significant. If the heterogeneity of the included literature is too high to conduct a meta-analysis, a descriptive analysis should be conducted.
Results
Literature Search Results
2228 relevant literature were initially retrieved and imported into the Note Express literature management software. After plagiarism check, 713 articles remained. After reading the titles and abstracts, 282 articles were selected for full-text evaluation, and finally 35 articles were included [1-36]. All of them are randomized controlled trials, and the literature screening process is shown in Figure 1.
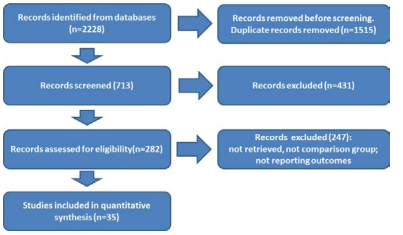
Figure 1: Identification of studies via databases and registers
Basic Characteristics
This study included 35 articles, with a total of 7965 cases of pediatric patients included. Among them, there were 4026 cases in the experimental group and 3939 cases in the control group.There were no statistically significant differences in baseline data such as gestational age, weight, age, and gender composition between the experimental and control groups (P>0.05), indicating comparability. The basic characteristics of the included literature are shown in Table 1.
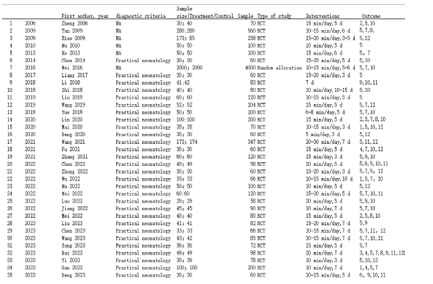
Table 1: Basic characteristics of the included literature. Indicate as: 1.Weight; 2.Sleep condition; 3.Neonatal neurobehavioral determination; 4.Crying; 5.Bilirubin levels and duration; 6.Hepatic function; 7.Defecation; 8.Breastfeeding condition; 9.The incidence of adverse reactions; 10.The time of stopping therapy and discharging; 11.Immune function, 12.Hospitalization rate or admission time.
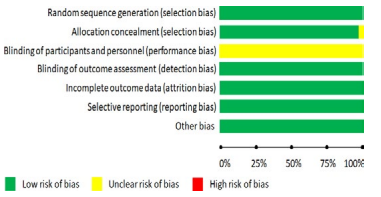
Figure 2: Bias risk assessment
Quality Assessment of Included Literature Among the 35 articles included, 34 of them used the random number table method. The articles only involved randomization but did not provide a detailed description of the randomization method, so the risk is unclear. All literature describes the predetermined outcome measures, therefore it is considered low-risk. There is no clear explanation in the literature regarding whether the allocation method is hidden and whether blinding is used, as bias is unclear. All studies have no other biases or selective reporting of results, indicating low-risk bias. The bias risk assessment chart is shown in Figure 2, and the scale chart is shown in Figure 3.

Figure 3: Bias Risk Ratio
Meta-Analysis Results
Total Efficiency: The total clinical efficacy rate of 17 articles was described, and heterogeneity test (I2=99%>50%,P<0.12) [4-6,13,14,16,19,20- 22,25,28,32-35]. There was some heterogeneity among the selected literature in this group. Random effects were selected for meta-analysis, and the results showed that in the treatment of neonatal jaundice, the combination of traditional Chinese medicine bath and conventional treatment had an advantage in total clinical efficacy rate compared to conventional treatment alone (RR=4.13, 95% CI (3.58, 5.69), Z=17.26, P<0.0001), as shown in Figure 4.
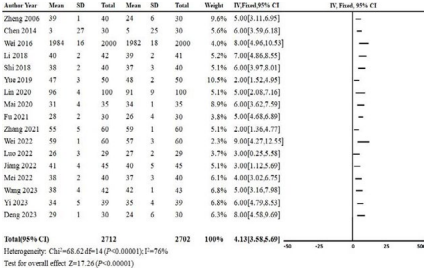
Figure 4: Meta-analysis of clinical efficacy rate
Bilirubin value analysis: The bilirubin value of 32 articles was described, and after heterogeneity testing (I2=99%>50%, P<0.1) [1-36]. It was found that there was some heterogeneity among the selected literature in this group. Random effects were selected for meta-analysis, and the results showed that in the treatment of neonatal jaundice, the combination of traditional Chinese medicine bath and conventional treatment had an advantage in reducing bilirubin levels compared to pure conventional treatment (SMD=-16.21, 95% CI (-21.19, -12.06), Z=55.26, P<0.0001), as shown in Figure 5.
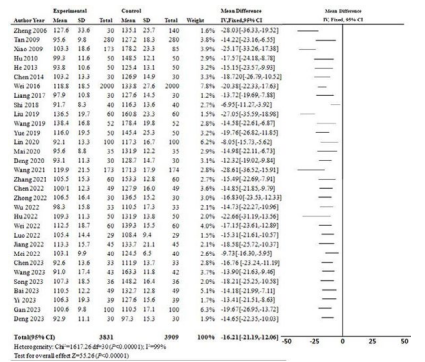
Figure 5: Meta-analysis of bilirubin values.
Analysis of Jaundice Resolution days: The duration of jaundice regression of 19 articles was described, and after heterogeneity testing. It was found that there was heterogeneity among the selected literature in this study [3-5, 7, 13, 14, 16, 19-22, 27-30, 32-35]. Random effects were selected for meta-analysis, and the results showed that in the treatment of neonatal jaundice, the combination of traditional Chinese medicine bath and conventional treatment alone can shorten the duration of jaundice regression compared to conventional treatment alone (SMD=8.29,95% CI (3.37,6.97), Z=27.65, P<0.0001), as shown in Figure 6.
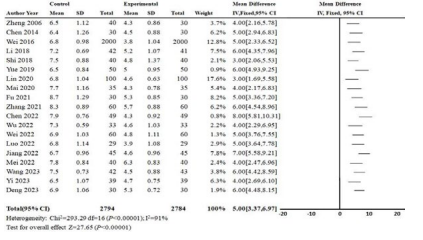
Figure 6: Meta-analysis of jaundice resolution days
Adverse Reaction Analysis: Adverse reactions of 5 articles were subjected to meta-analysis. After heterogeneity testing, it was found that there was significant heterogeneity among the selected literature in this study [3,14,19,34,36]. Random effects were selected for meta-analysis, and the results showed that there was no significant difference in the incidence of adverse reactions between traditional Chinese medicine bath combined with conventional treatment and conventional treatment alone in the treatment of neonatal jaundice [RR=0.73, 95% CI (0.15, 0.58), Z=0.27, P>0.05], as shown in Figure 7.
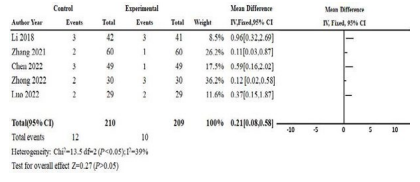
Figure 7: Publication Bias of Clinical Efficacy Rate
Publication Bias Analysis
In this study, the main outcome measures (clinical total response rate, post-treatment serum total bilirubin level) were used to draw a funnel plot to evaluate bias, which can better and comprehensively observe the degree of publication bias. From the funnel plots of clinical total effective rate (Figure 8) and post-treatment serum total bilirubin (Figure 9), it can be observed that the studies on both sides of the funnel are asymmetric, indicating that there may be some publication bias in this study. Exploring the reasons, the following aspects may cause this bias: (1) This study extensively searched for literature on the treatment of neonatal jaundice with traditional Chinese medicine baths, but there were basically no negative results published in this study, all of which were positive results; (2) Most of the studies included in this study have small sample sizes and generally low quality. (3) In this study, all the included literature is in Chinese, so there may be some language publication bias.
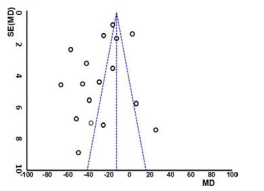
Figure 8: Clinical total effective rate.
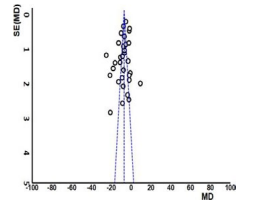
Figure 9: Publication bias of serum bilirubin value.
Discussion
This study comprehensively searched for literature on the treatment of neonatal jaundice with traditional Chinese medicine baths in China over the past 30 years, and ultimately included 35 studies. The results of the systematic evaluation analysis show that: (1) In terms of clinical total effective rate, 17 studies reported clinical total effective rate, with a total of 5414 children, 2712 in the treatment group and 2702 in the control group. The meta-analysis results showed P<0.05, which is statistically significant, indicating that the combination of traditional Chinese medicine bath and conventional treatment has a significant advantage in overall clinical efficacy compared to conventional treatment. (2) In terms of bilirubin levels, 32 studies reported serum total bilirubin levels, including 7740 children, 3831 in the treatment group and 3909 in the control group. The meta-analysis results showed P<0.05, which is statistically significant, indicating that the combination of traditional Chinese medicine bath and conventional treatment has a significant advantage in serum bilirubin levels compared to conventional treatment. (3) In terms of the number of days of jaundice regression: A total of 19 studies reported the number of days of jaundice regression, including 5578 children, 2784 in the treatment group and 2794 in the control group. The meta-analysis results showed P<0.05, which is statistically significant. It suggests that in the treatment of neonatal jaundice, the combination of traditional Chinese medicine bath and conventional treatment can shorten the number of days of jaundice regression compared to pure conventional treatment. (4) In terms of adverse reactions: A total of 5 studies reported adverse reactions, including 419 children, with 210 in the control group and 209 in the treatment group. Meta-analysis results showed P>0.05, which is statistically significant. The results suggest that in the treatment of neonatal jaundice, the combination of traditional Chinese medicine bath and conventional treatment has no significant difference in the incidence of adverse reactions compared to Western medicine conventional treatment alone. Therefore, existing evidence suggests that in the treatment of neonatal jaundice, the combination of traditional Chinese medicine bath and conventional treatment has significant advantages over conventional treatment alone in terms of overall clinical efficacy, total bilirubin levels after treatment, and jaundice resolution days. From the screening and inclusion of literature in this study, it can be seen that a large number of randomized controlled trials (RCTs) have been conducted in China using traditional Chinese medicine baths as intervention measures for the treatment of neonatal jaundice, and the number of published literature has been increasing year by year, indicating that the use of traditional Chinese medicine baths for the treatment of neonatal jaundice has gradually gained attention and recognition. This study selected literature with Jadad scores ≥ 3 and strictly screened the literature according to inclusion and exclusion criteria. However, there are still the following limitations: (1) In terms of literature quality: 1) Randomization concealment: None of the literature described randomization concealment. 2) Blinding method: None of the literature selected for this study explicitly reported the use of blinding during the research process Withdrawal and loss to follow-up: None of the literature mentioned whether any cases withdrew or were lost to follow-up during the research process. (2) The literature included in this study showed differences in the composition and dosage of medicinal baths, the duration of traditional Chinese medicine baths, and the treatment course. Additionally, the control group had different conventional Western medicine treatment methods, which increased the possibility of heterogeneity. (3) The literature included in this study did not have any English literature with certain language publication bias, and the results of this study were all positive, which may also have some publication bias. (4) Only a small number of literature included in this study reported adverse reactions caused by traditional Chinese medicine baths, but did not provide detailed records of the specific manifestations and duration of adverse reactions. Moreover, this study did not mention whether follow-up and recurrence rates were available, which led to the failure of this systematic review to clearly indicate the safety of traditional Chinese medicine baths in treating neonatal jaundice. Through meta-analysis, it has been confirmed that the combination of traditional Chinese medicine bath and conventional treatment has advantages over conventional treatment alone in the treatment of neonatal jaundice in terms of overall clinical efficacy, total bilirubin levels after treatment, and jaundice resolution days. The use of medicinal bath in the treatment of neonatal jaundice can be applied and promoted in clinical practice. However, due to the lack of standardized clinical research methods, the literature included in this study is of low quality, and more high-quality, double-blind randomized controlled trials are needed for validation in the future.
Funding Sources
This work was supported by grants from Traditional Chinese Medicine Treatment Advantage Disease Project (10000015Z155080000004) to YY.
Acknowledgement
None.
Conflict of Interest Statement
There is no conflict of interest for authors.
Ethics Approval Statement
Not applicable.
References
1. Bai, G., et al. (2023). Observation on the therapeutic efficacy of bath with Yinling Jianpi Tuihuang decoction combined with bifidobacterium live bacteria in the treatment of neonatal jaundice. Journal of Changchun University of Chinese Medicine, 39, 1246-1250.
2. Chen, K., et al. (2023). The therapeutic effect of blue light therapy combined with traditional Chinese medicine fumigation and washing combined with refined nursing on neonatal jaundice. Modern Medicine and Health Research, 7, 132-134.
3. Chen, L., et al. (2022). Clinical effect of herbal fumigation of Jianghuang powder combined with blue light irradiation on neonatal jaundice. Clinical Research and Practice, 7, 134- 136.
4. Chen, Q., et al. (2014). Observation ofthecurativeefectoftraditionalChinesemedicinebath combined with massage inthetreatmentofneonatalpathologicjaundicein 30 Cases. ChineseYoujiangMedical Journa, 42, 641-643.
5. Deng, J., et al. (2023). Clinical Observation of Chinese Medicine Bath Combined with Yinzhihuang Oral Liquid in the Treatment of Neonatal Jaundice and the Effect of Intervention on Immune Function. Drug Evaluation, 20, 705-708.
6. Deng, W., et al. (2020). Application of traditional Chinese medicine bath combined with blue light irradiation and Bacillus subtilis dual live bacteria particles in the treatment of neonatal jaundice. Medical Equipment, 33, 75-76.
7. Fu, J., et al. (2021). Efficacy of Herbal Bathing on Neonatal ABO Hemolytic Jaundice and Anemia. Clinical Journal of Chinese Medicine, 33, 1326-1329.
8. Gan, L., et al. (2023). Effect of Chinese herbal medicatedbath combined with infantile massage on total bibirubin and traditional Chinese medicine syndrome in fetal jaundice with syndrone of stagnation and steaming of damp-heat. Hebei J TCM, 45, 1445-1448.
9. He, J. (2013). The effect of traditional Chinese medicine bath combined with abdominal touch on neonatal jaundice. Journal of Qilu Nursing, 19, 86-87.
10. Hinkal, G. W., et al. (2009). Altered senescence, apoptosis, and DNA damage response in a mutant p53 model of accelerated aging. Mech Ageing Dev, 130, 262-71.
11. Hu, C. (2022). Effect of Yinchenhao Decoction Bath Combined with Intermittent Blue Light Irradiation in the Treatment of Neonatal Jaundice. Chinese and Foreign Medical Research, 20, 136-140.
12. Hu, X., et al. (2011). The effect of Huangbai external washing on neonatal bilirubin levels. Journal of External Therapy of Traditional Chinese Medicine, 20, 37.
13. Jiang, W., et al. (2022). Clinical Observation on External Washing Combined with Acupoint Massage in the Treatment of Neonatal Pathological Jaundice. Chinese Medicine Modern Distance Education of China, 20, 95-96.
14. Li, L. (2018). Effect of Chinese herbal bath on serum transferrin and C-reactive protein in neonatal jaundice. Shaanxi Journal of Traditional Chinese Medicin, 39, 443-445.
15. Liang, Z., et al. (2017). Clinical effect of novel Chinese medicine of neonatal Tuihuang lotion on jaundice neonates with G-6PD deficiency. Guangxi Medical Journal, 39, 450- 452.
16. Lin, X., et al. (2020). Clinical observation on the comprehensive treatment of neonatal pathological jaundice with meridian massage combined with traditional Chinese medicine bath. Chinese Journal of Traditional Medical Science and Technology, 27, 908-909.
17. Liu, L. (2023). Observation on the therapeutic effect of Bacillus subtilis combined with traditional Chinese medicine fumigation and washing on neonatal jaundice. Journal of North Pharmacy, 20, 174-176.
18. Liu, Y., et al., 2019. Observation of the therapeutic effect of blue light therapy combined with traditional Chinese medicine bath on neonatal jaundice. Chinese Journal of Integrated Traditional and Western Medicine on Liver Diseases. 29, 374- 375.
19. Luo, C. (2022). Clinical Observation on Chinese Medicine External Washing Combined with Bifidobacterium Triple Viable Powder in the Treatment of Neonatal Jaundice. Chinese Medicine Modern Distance Education of China, 9, 131-133.
20. Mai, X., et al. (2020). Therapeutic Effectiveness of Tmmtional Chininese Medicine Soaking and Washing in the Newborn Jaundice. Journal of Liaoning University of TCM, 22, 207- 210.
21. Mei, M., et al. (2022). Clinical efficacy of Traditional Chinese Medicine bath with self-designed Tuihuangfang decoction combined with acupoint massage and blue light irradiation in the treatment of neonatal pathological jaundice. Contemporary Medicine, 28, 154-156.
22. Shi, Y., et al. (2018). Observation on Clinical Effects of Traditional Chinese Medicine Prescriptions for External Wash in Treating Neonatal Jaundice. Western Journal of Traditional Chinese Medicine, 31, 112-114.
23. Song, H., et al. (2023). The Application of Chinese Medicine Bath Combined with Chiropractic in the Nursing of Neonatal Jaundice. Guangming Journal of Chinese Medicine, 38, 4675- 4678.
24. Tan, G., et al. (2009). Golden Dragon Chinese medicine bag to prevent and treat physiological jaundice of new born. J. PEDIATRICS OF TCM, 5, 25-28.
25. Wang, L., et al. (2023). Clinical efficacy of anti -jaundice formulas with massage for neonatal pathological jaundice with blood stasis and amassment and its effects on bilirubin and inflammatory index Hebei J TCM, 45, 56-60.
26. Wang, M., et al. (2019). Clinical Observation on Oral Administration of Yinchen Granules Joined with Herbal Fumigation in the Treatment for Neonatal Pathological Jaundice. Western Journal of Traditional Chinese Medicine, 32, 116-118.
27. Wang, Y. (2021). Clinical observation on treating 347 cases ofneonatal jaundice by infantile massage plus TCM medicine fumigation-washing therapy. Clinical Journal of Chinese Medicine, 13, 128-131.
28. Wei, N., Wei, T. (2022). Effect of Yinzhihuang Decoction Bath Combined with Touch Nursing on Neonatal Jaundice. Journal of Sichuan of Traditional Chinese Medicine, 40, 214- 216.
29. Wei, Y., et al. (2016). Study on the Effect of Chinese Medicine Bath Combined with Five Elements Music Therapy on Neonatal Jaundice. Mod Diagn Treat, 17, 3158-3159.
30. Wu, H., et al. (2022). Clinical efficacy of blue light irradiation combined with probiotics and traditional Chinese medicine bath in the treatment of neonatal jaundice. Heilongjiang Medicine and Pharmacy, 45, 62-64.
31. Xiao, D., et al. (2009). The preventive effect of traditional Chinese medicine bath combined with sun exposure on neonatal jaundice. Chinese Medicine Modern Distance Education of China, 3, 19.
32. Yi, H., et al. (2023). Clinical observation on the treatment of neonatal jaundice with traditional Chinese medicine soaking and washing combined with blue light irradiation and riboflavin. Guangming Journal of Chinese Medicine, 38, 4648-4651.
33. Yue, X., et al. (2019). Observation on Clinical Effects of Medicated Bath of Tuihuang Waixi Prescription in Early Intervention for Neonatal Jaundice. Western Journal of Traditional Chinese Medicine, 32, 68-70.
34. Zhang, W., et al. (2021). Clinical Study on Chinese Herbal Fumigation and Washing Combined with Blu-Ray Irradiation and Combined B. Subtilis and E. Faecium Granules with Multivitamines, Live for Neonates with Pathological Jaundice. Journal of New Chinese Medicine, 53, 89-90.
35. Zheng, C. (2006). Therapeutic Effectiveness of Herb Soaking and Washing in the Adjuvant Treatment of Infant Jaundice. Journal of Nursing Science, 21, 29.
36. Zhong, L., et al. (2022). Effect of Bacillus Subtilis combined with traditional Chinese medicine immersion (fumigation) on neonatal jaundice. China Modern Medicine, 29, 64-66.



