Case Report - (2023) Volume 8, Issue 6
Successful Surgical Treatment of Anterior Fusion Cage Dislocation into the Cervical Esophagus
Received Date: Jun 05, 2023 / Accepted Date: Jun 12, 2023 / Published Date: Jun 13, 2023
Abstract
We report on a 50-year-old patient’s case, who underwent ventral and dorsal cervical fusion for polytrauma due to car accident. The patient suffered very rare complication of the surgery-cage dislocation into the cervical esophagus. He underwent multiple surgical interventions: ventral and dorsal cervical fusion, laminectomy, tracheostomy, epicystostomy, gastrostomy. The surgical treatment was divided into two stages. At the first stage, open cholecystectomy and gastrostomy correction were performed and at the second stage, extraction of the cage and closure of the esophageal wall defect were performed. To prevent failure of the sutures placed on the wound of the esophagus, the method of covering the suture line with a pedicled flap cut from the medial portion of the sternocleidomastoid muscle was used. The control X-Ray examination was performed at 6th p/o day, which reveals no extravasation and free passage of contrast to the stomach. The patient after almost a three-year break began peroral eating and was discharged the hospital at 10th p/o day. We consider, that the method of covering the suture line by pedicled flap from sternocleidomastoid muscle in cases of difficult suturing of defects of the cervical esophagus, is a good surgical option. Surgeons should be aware of the risk of cage dislocation of cervical fusion procedure.
Keywords
Cage dislocation, Esophageal defect, Pedicled muscle flap, Endoscopy, Dysphagia, Laminectomy, Tracheostomy, Epicystostomy, Gastrostomy
Introduction
At the present time the ventral and dorsal cervical fusion is a common surgical procedure for treatment of cervical vertebral instability. A variety of implant-related short and long-term complications after fusion surgery are recognized. Mid to longterm complications due to cage migration and/or cage subsidence are less frequently reported and esophageal perforation is a rare but well-known complication of anterior cervical spine surgery [2,7,9-20]. We present a very rare case of delayed cage dislocation into the cervical esophagus, and surgical intervention was taken to remove it. In the available literature there were rarely similar cases with multiple surgical interventions and surgical removal of dislocated cage and primary repair of the defect of esophagus.
Case Report
A 50-year-old male patient presented with dysphagia, neck pain, globus sensation and inability to swallow saliva and complete immobility of the lower limbs. From his past medical history, it became known that 3 years ago after the car accident and due to polytrauma with traumatic spinal cord injury in another hospital he underwent multiple surgical interventions: ventral and dorsal cervical fusion, laminectomy, tracheostomy, epicystostomy, gastrostomy. He was held long-term inpatient (resuscitation) treatment with diagnosis: C6 compression fracture with traumatic myelopathy, skull-valve fracture, focal brain injury, skull base fracture, scalp open wound, multiple rib fractures, traumatic hemopneumothorax, acute shortness of breath, pneumonia, acute peritonitis, dysphagia, tetraplegia. During this period of time, he underwent also removal of the ventral plate due to dislocation into the cervical esophagus with repair of defect of esophageal wall, which was complicated by leakage and abscess formation. The abscess debridement and closure of the defect with a skin flap was performed. The instrumental studies (Endoscopy, CT) performed in our hospital revealed the following clinical picture: anterior cage dislocation into the cervical esophagus (Figure 1,2). Taking into account the above complaints, the data of the performed studies and the possibility of developing serious complications (primarily esophageal perforation with subsequent mediastinitis) the additional surgical revision was recommended.
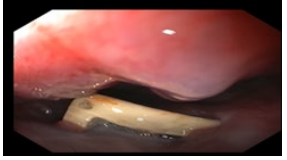
Figure 1: Preoperative Endoscopy View.
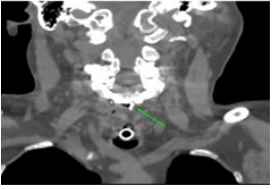
Figure 2: Preoperative CT Data

Figure 3: Removal of dislocated cage
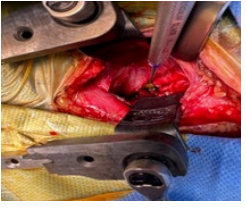
Figure 4: Defect of esophagus.
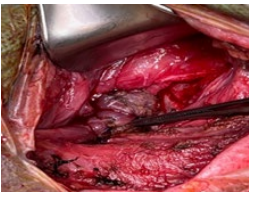
Figure 5: Covering the suture line by pedicled scm flap
Operative Treatment
The surgical treatment was divided into two stages because of multiple medical comorbidities. At the first stage, open cholecystectomy and gastrostomy correction were performed taking into account the patient’s condition and multiple interventions to form a gastrostomy. After 3 weeks at the second stage, extraction of the cage and closure of the esophageal wall defect were performed. A longitudinal incision was made along the medial margin of the left sternocleidomastoid muscle for expose of operative field and the neurosurgeon’s team have performed the cage extraction. After this part of the operation, a defect of left and posterior wall of cervical esophagus up to 2 cm long was revealed. The repair of esophageal defect in one layer by using interrupted sutures was performed above naso-gastric tube. It was technically impossible to perform a double-row suture due to the tight fixation of the posterior wall of the esophagus to the prevertebral fascia. To prevent the leakage the method of covering the suture line by pedicled flap from sternocleidomastoid muscle was used (Figure 3-5). The SCM flap was first demonstrated by Jianu in 1882 as the treatment of choice for facial paralysis, nowadays, it can be used for various purposes [23]. Vacuum drainage of the surgical wound completed the surgical intervention. Multimodal opioid free anesthesia technique was done, which provides excellent anesthesia and analgesia.
Results
Postoperative course was uneventful and without complications. The control X-Ray examination was performed at 6th p/o day, which reveals no extravasation and free passage of contrast to the stomach (Figure 6). The patient after almost a three-year break began peroral eating and was discharged the hospital at 10th p/o day. After 1 month of surgery the patient is doing well, undergoing rehabilitation course, eats liquid and semi-liquid food and does not show any additional complaints.

Figure 6: Control X-Ray at 6th p/o day.
Discussion
Delayed pharyngoesophageal perforation is a rare complication following anterior cervical spine surgery [9-15]. The unique anatomy of the anterior neck presents a wide variety of potential complications involving vascular, aerodigestive, neural, and osseous structures, in which esophageal perforation was found in 0.2% of cases [16-20]. The mechanism and causes of development of cage migration and dislocation are still unclear and the risk factors are not well understood. Gragnaniello et al. reported that possible causes of the anterior dislocation of the Maverick prosthesis include the following: 1) surgeon error; 2) equipment problem; 3) prosthesis fault and 4) patient factors [5]. Hua et al. revealed that less than 3 years of surgeons’ experience, small cage size, and lumbar spondylolisthesis were independently associated with cage migration [6]. Duncan and Bailey have concluded that unilateral fixation is not stable enough to prevent fusion cage migration in some patients who undergo transforaminal lumbar interbody fusion [3]. Leute and al. have concluded that Hardware-related complications are rarely seen in patients with open transforaminal lumbar interbody fusion, but must be kept in mind and can potentially cause severe neurological deficits. Aoki et al., reported that the potential for postoperative cage migration and limitations of unilateral fixation should be considered by spine surgeons [7,8]. The rates of complications for dysphagia, esophageal perforation, and graft or hardware failure were 5.3 ï¼?, 0.2ï¼?, and 2.1ï¼? respectively [15,16]. Halani et al. after systematic review of 65 articles with 153 patients (mean age 44.7 years; range 14-85 years) who underwent anterior spinal surgery and sustained esophageal perforation have concluded, that esophageal perforation after anterior cervical spine surgery is a rare complication which can have significant morbidity and mortality (3.92%) [17-19]. These perforations can be stratified into 3 categories based on the timing of symptomatic onset: intraoperative, early postoperative (within 30 days of anterior spinal surgery), and delayed. Delayed presentation of a perforation has been reported in 0.2 to 1.5% of cases and average time to diagnosis was 2 years [17,18]. Rueth et al. reported that cases of esophageal perforation may be discovered intraoperatively, or even as late as 10 years after surgery [22]. The most common source of esophageal injury is hardware erosion or migration, each of which may vary in their time to symptomatic manifestation [17-19]. There is no consensus to the optimal management of these patients in the literature. Many authors recommend as the first option of treatment: intravenous broad-spectrum antibiotics therapy, removal of hardware and early surgical closure of the defect supported with a vascularized flap. At reconstruction for reinforcement of the esophageal perforation repair a sternocleidomastoid (SCM) flap was the most common choice, while a pectoralis flap was used in cases where the initial SCM flap had failed or the esophageal perforation was too large and inability to reapproximate mucosal flaps without excessive tension [17,18,21]. Oral intake should be forbidden and nasogastric tube or gastrostomy must be conducted for nutrition support [9-11,17]. So, the review of literature shows that esophageal perforation following anterior cervical spine surgery is a challenging clinical problem for the surgeons and our case, which is described above, fully confirms this assumption.
Conclusion
Our case illustrates, that the cage removal and primary esophageal repair is the best radical treatment strategy in cases of cage dislocation with esophageal perforation. The using of sternocleidomastoid pedicled muscle flap to reinforce primary closure of the cervical esophageal defect to prevent the postoperative leakage and achieve successful outcome is the most optimal and effective surgical option in this situation. A multidisciplinary team approach is essential in the treatment of these complex surgical patients.
References
1. Leute, P.J., Hammad, A., Hoffmann, I., Hoppe, S., Klinger, H.M., et al. (2015). Set screw fracture with cage dislocation after two-level transforaminal lumbar interbody fusion (TLIF): a case report. J Medical Case Reports, 9, 22.
2. Corniola, M.V., Jägersberg, M., Stienen, M.N., Gautschi, O.P. (2015). Complete cage migration/subsidence into the adjacent vertebral body after posterior lumbar interbody fusion. Journal of clinical neuroscience: official journal of the Neurosurgical Society of Australasia, 22(3), 597-598.
3. Duncan, J.W., Bailey, R.A. (2013). An analysis of fusion cage migration in unilateral and bilateral fixation with transforaminal lumbar interbody fusion. European Spine Journal, 22(2), 439-445.
4. Oh, H.S., Lee, S.H., Hong, S.W. (2013). Anterior dislodgement of a fusion cage after transforaminal lumbar interbody fusion for the treatment of isthmic spondylolisthesis. Journal of Korean Neurosurgical Society, 54(2), 128-131.
5. Gragnaniello, C., Seex, K.A., Eisermann, L.G., Claydon, M.H., Malham, G.M. (2013). Early postoperative dislocation of the anterior Maverick lumbar disc prosthesis: report of 2 cases. Journal of Neurosurgery Spine, 19(2), 191-196.
6. Li, H., Wang, H., Zhu, Y., Ding, W., Wang, Q. (2017). Incidence and risk factors of posterior cage migration following decompression and instrumented fusion for degenerative lumbar disorders. Medicine, 96(33), e7804.
7. Aoki, Y., Yamagata, M., Nakajima, F., Ikeda, Y., Takahashi, K. (2009). Posterior migration of fusion cages in degenerative lumbar disease treated with transforaminal lumbar interbody fusion: a report of three patients. Spine, 34(1), E54-E58
8. Aoki, Y., Yamagata, M., Nakajima, F., Ikeda, Y., Shimizu, K., et al. (2010). Examining risk factors for posterior migration of fusion cages following transforaminal lumbar interbody fusion: a possible limitation of unilateral pedicle screw fixation. Journal of neurosurgery. Spine, 13(3), 381- 387.
9. Hanci, M., Toprak, M., Sarioglu, A.C. (1955). Oesophageal perforation subsequent to anterior cervical spine screw/ plate fixation. Paraplegia, 33, 606-609.
10. Phommachanh, V., Patil, Y.J., McCaffrey, T.V., Vale, F., Freeman, T.B., et al. (2010). Otolaryngologic management of delayed pharyngoesophageal perforation following anterior cervical spine surgery. The Laryngoscope, 120(5), 930-936.
11. Lu, X., Guo, Q., Ni, B. (2012). Esophagus perforation complicating anterior cervical spine surgery. Eur Spine J, 21(1), 172-177.
12. Hu, L.S.h., Wu, Z.Q., Zou, L.M., Huang, Y.C. (2019). The treatment of esophageal perforation after anterior cervical spinal surgery. Case Reports in Surgery, 2019, 2350958.
13. Orlando, E. R., Caroli, E., & Ferrante, L. (2003). Management of the cervical esophagus and hypofarinx perforations complicating anterior cervical spine surgery. Spine, 28(15), E290-E295.
14. Dakwar, E., Uribe, J.S., Padhya, T.A., Vale, F.L. (2009). Management of delayed esophageal perforations after anterior cervical spinal surgery. Journal of Neurosurgery Spine, 11(3), 320-325.
15. Yeh, M.Y., Huang, W.C., Kuo, C.H., Chang, P.Y., Cheng, H. (2019). Disappearance of Anterior Cervical Corpectomy Cage. Cureus, 11(1), e3985.
16. Yee, T.J., Swong, K., Park, P. (2020). Complications of anterior cervical spine surgery: a systematic review of the literature. J Spine Surg, 6, 302-322.
17. Halani, S.H., Baum, G.R., Riley, J.P., Pradilla, G., Refai, D., et al. (2016). Esophageal perforation after anterior cervical spine surgery: a systematic review of the literature. J Neurosurgery Spine, 25(3), 285-291.
18. Lee, T.S., Appelbaum, E.N., Sheen, D., Han, R., Wie, B. (2019). Esophageal Perforation due to Anterior Cervical Spine Hardware Placement: Case Series. Int J Otolaryngology, 7682654.
19. Kang, M.S., Kim, K.H., Park, J.Y., Kuh, S.U., Chin, D.K., et al. (2017). Management of Esophageal and Pharyngeal Perforation as Complications of Anterior Cervical Spine Surgery. World Neurosurgery, 102, 275-283.
20. Dantas, F.R., Dantas, F., Mendes, P.D. (2020). Primary Repair of Esophageal Perforation Following Anterior Cervical Fusion. Cureus, 12(11), e11590.
21. Ahn, S.H., Lee, S.H., Kim, E.S., Eoh, W. (2011). Successful repair of esophageal perforation after anterior cervical fusion for cervical spine fracture. J Clin Neurosci, 18(10), 1374-1380.
22. Rueth, N., Shaw, D., Groth, S., Stranberg, S., D’Cunha, J., et al. (2010). Management of cervical esophageal injury after spinal surgery. The Annals of thoracic surgery, 90(4), 1128-1133.
23. Fatani, B., Alabood, A.A., Alkhayatt, NM., et al. (2023). Facial Reconstruction Using Sternocleidomastoid (SCM) Flap: A Review of the Literature. Cureus, 15(2), e34575.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



