Case Report - (2023) Volume 8, Issue 5
Skull Base Chordoma: About Two Cases and Literature Review
Received Date: Mar 13, 2023 / Accepted Date: May 08, 2023 / Published Date: May 15, 2023
Abstract
Skull base chordomas are rare primitive bone tumors developed at the expense of remnants of the embryonic notochord at the level of the clivus, characterized by invasive behavior at the local level with possibility of extension to neighbouring organs. The deep localization of these tumors and their proximity to the structures of the base of the skull round a carcinological resection difficult if not impossible. Radiation therapy, both adjuvant to surgery and exclusive, is a therapeutic approach to improve local control and quality of life for patients. We present two cases of patients followed for skull base chordoma treated with exclusive radiotherapy.
Keywords
Chordoma, Skull Base, Radiotherapy.
Case Presentation
Case 1
The first case is a 54-year-old patient, who has had intense headaches and visual disturbances for the past four months. Brain MRI showed the presence of a tumor process centered on the left lateralized sphenoidal bone, invading the petrified apex, the carotid canal, infiltrating the upper orbital fissure with extension to the infra-temporal fossa (Figure 1).
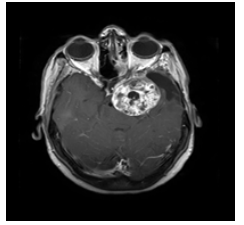
Figure 1: Brain MRI in axial section showing the tumor process.
A biopsy with immunohistochemical complement of the sphenoid sinus was in favor of a chondroid chordoma: Anti EMA+, Anti PS 100+, Anti CKAE1/AE3+. Surgery was recused due to the complex localization of the tumor, and the patient was treated with radiotherapy at a dose of 60Gy in 2Gy per fraction for a 40-day spread. The irradiation was done by VMAT technique, using two arcs. Analysis of the dose-volume histogram showed good coverage of target volumes with dose constraints acceptable for organs at risk (figure 2). At 10 months from the end of treatment, the evolution was marked by a significant regression in the lesion process on the MRI.

Figure 2: Target volume and dose volume histogram for patient 1.
Case 2
The second case is a 60-year-old patient with no previous history who has had severe back-ear pain and headache with dizziness for the past six months. Brain MRI was in favor of a lesional process of the left ponto-cerebellar angle with significant extension to the rock and mastoid, and is responsible for a mass effect on the brainstem and fourth ventricle. The biopsy with immunohistochemical supplement has returned in favor of a chordoma N.O.S: Anti EMA +, Anti PS 100+, Anti AE1/AE3+, Anti vimentine+, Anti Brachyurie+. Surgery was not possible and the patient was treated with VMAT radiation at a dose of 60 Gy in 2 Gy per fraction over 42 days (Figure 3). At 06 months from the end of the treatment, the evolution was marked by lesion radiological stability on MRI.
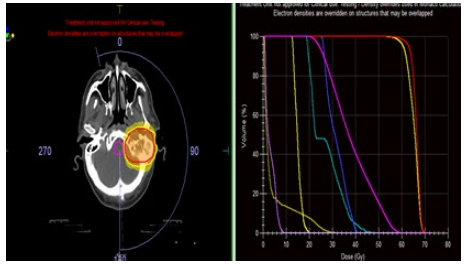
Figure 3: Target volume and dose volume histogram for patient 2
Discussion
Skull base chordomas are very rare extra-axial tumors representing less than 0.2% of intracranial tumors [1]. These tumors originate from the remnants of notochord [2], and arise from the clivus.
They can be seen in all age groups, but the majority of cases are diagnosed in person in the fifth and sixth decades of life [2]. The gender distribution has been reported to be nearly equal in the skull base lesions.
Clinical symptomatology is non-specific, and mainly depends on the location, size and extension to nearby structures. Neuroophthalmologic signs are most frequently encountered; visual field alteration, ptosis, diplopia. Headaches can also be observed reflecting a dural direct invasion, a compression of the trigeminal nerve or intracranial hypertension.
The high-resolution scanner with bone and parenchymal windows allows an evaluation of the importance of bone destruction and invasion. The chordoma takes on the appearance of an expansive osteolytic tumor centered on the clivus, extended to adjacent tissue [3]. Intratumor microcalcifications reflect bone destruction. MRI is the exam of choice, allowing an accurate description of the tumor weighted images (T1WI) [4], and heterogeneous hypersignal in T2-weighted images (T2WI) [5].
Contrast taking after gadolinium injection reflects aggression and the risk of recurrence or progression after surgery [6]. Surgery is the angular part in the support of chordoma. The purpose of this surgery is the complete removal of the tumor with negative resection margins. However due to the deep localization and proximity to neurological structures, this excision is impossible. A subtotal resection can be discussed to reduce the risk of neurological sequelae.
Radiotherapy plays a major role in the management of chordoma. Both postoperatively in the event of residual tumor or as exclusive treatment in the event of inoperable disease, it certainly also finds indications as an adjuvant to complete resection in the event of poor prognostic factors.
A dose-response relationship exists in the treatment of chordomas by radiotherapy. The probability of recurrence of chordomas depends on the level of homogeneity of the dose delivered to the target volume.
Proton therapy and carbon ions deliver high doses to the tumor while sparing nearby organs. Proton therapy makes it possible to increase the dose in the tumor and to spare the surrounding critical organs as much as possible thanks to the ballistic characteristics of the protons [7]. This physical feature is fundamental to explain the dose gradient that can be obtained near a critical organ. The dose varies from 10 to 15% per millimeter of tissue crossed [8]. It was then shown that local control was improved and the risk of toxicity acceptable in a large number of series. This is why, for several years, proton irradiation has become the reference irradiation technique in the management of chordomas of the base of the skull after surgery [8].
A unique property of carbon ions compared to proton beams is their high biological efficiency. The relative biological effectiveness of carbon ions is estimated to be 1.5 to 3 times greater than that of photons, electrons and even protons. These physical qualities of carbon ions would partly explain their excellent results in the treatment of chordomas [9].
Innovative photon radiotherapy techniques in IMRT and VMAT would be an alternative to hadrontherapy and comparative studies between the different techniques are necessary although difficult to set up. Intensity-modulated radiotherapy delivers a homogeneous dose in the target volume, thus allowing an increase in the dose delivered to the tumor by reducing the dose to neighboring healthy tissue. The recommended doses range from 56 to 70Gy.
Stereotactic radiotherapy is also a promising technique, allowing control of the pathology comparable to proton therapy thanks to an increase in the dose prescription while decreasing the frequency of adverse effects [10].
In general, chordoma are chemoresistant tumors, and there is no evidence to support cytotoxic chemotherapy in the treatment. A phase II prospective study using chemotherapy did not show positive results [11]. Several therapeutic protocols have been studied. Dhall et al. evaluated ifosfamide and etoposide in 6 children followed for a chordome of the base of the skull in a retrospective trial: Four out of 6 patients were alive, with stable radiographic abnormalities at median follow-up 9 years from diagnosis [12]. Also imatinib alone or combined with sirolimus has shown some efficacy in terms of local control in PDGFexpressing chordomas [13,14].
Patient survival depends more on local disease progression than metastasis. Local recurrence is the most important predictor of mortality and extension of the resection the best local control factor. Close follow-up is essential to detect and treat recurrences early [15].
Conclusion
Skull base Chordoma is a rare malignant tumor with a high risk of local and locoregional recurrence, on the other hand metastases are late. Surgery is the main therapeutic weapon to ensure local control. Adjuvant or exclusive radiotherapy retains a major place in the management of this disease.
References
1. Lee, S. Y., Lim, Y. C., Song, M. H., Seok, J. Y., Lee, W. S., & Choi, E. C. (2005). Chondrosarcoma of the head and neck. Yonsei Medical Journal, 46(2), 228-232.
2. McMaster, M. L., Goldstein, A. M., Bromley, C. M., Ishibe, N., & Parry, D. M. (2001). Chordoma: incidence and survival patterns in the United States, 1973-1995. Cancer Causes & Control: CCC, 12(1), 1-11.
3. Schamschula, R.G., & Soo, M.Y. (1993). Clival chordomas. Australas Radiol, 37(3), 259-264.
4. Sze, G., Uichanco, 3rd L.S., Brand-Zawadzki, M.N., et al. (1998). Chordomas: MR Imaging. Radiol, 166, 187e191.
5. Meyers, S.P., Hirsch, Jr W.L., Curtin, H.D., Barnes, L., Sekhar, L.N., & Sen, C. (1992). Chordomas of the skull base: MR features. AJNR Am J Neuroradiol, 13, 1627e1636.
6. Lin, E., Scognamiglio, T., Zhao, Y., Schwartz, T.H., & Phillips, C.D. (2018). Prognostic implications of gadolinium enhancement of skull base chordomas. AJNR Am J Neuroradiol, 39, 1509e1514.
7. Georgea, B., Bresson, B., Bouazza, S., Froelich, S., Mandonnet, E., & Hamdi, S. et al. (2014). Les chordomes. Neurochirurgie, 60(3), 63-140.
8. Brada, M., Pijls-Johannesma, M., & De Ruysscher, D. (2007). Proton therapy in clinical practice: current clinical evidence. Journal of clinical oncology: official journal of the American Society of Clinical Oncology, 25(8), 965-970.
9. Imai, R., Kamada, T., Tsuji, H., Sugawara, S., Serizawa, I., & Tsujii, H., et al. (2010) Effect of Carbon Ion Radiotherapy for Sacral Chordoma: Results of Phase I-II and Phase II Clinical Trials. Int J Radiat Oncol, 77(5), 1470â?1476.
10. Batchinsky-Parrou, V., Hemery, C., Delemer, Brig., & Litré, Claude Fabien. (2020). Traitement des chordomes du clivus par approche combinée : chirurgie et radiothérapie stéréotaxique VMaT. À propos de 17 cas. Annales d’Endocrinologie, 81, 169.
11. Chugh, R., Dunn R, Zalupski, M.M., et al. (2005). Phase II study of 9-nitrocamptothecin in patients with advanced chordoma or soft tissue sarcoma. J Clin Oncol, 23, 3597e3604.
12. Dhall, G., Traverso, M., Finlay, J.L., et al. (2011). The role of chemotherapy in pediatric clivalchordomas. J Neurooncol, 103:657e662.
13. Silvia, S., Alessandra, L., Virginia, F., Giovanni, G., Alessandro, C., & Roger Stupp, et al. (2012) Phase II study of imatinib in advanced chordoma. J Clin Oncol, 30(9), 914-920.
14. Stacchiotti, S., Marrari, A., Tamborini, E., Palassini, E., Virdis, E., Messina, A., et al. (2009) Response to imatinib plus sirolimus in advanced chordoma. Ann Oncol 20(11), 1886-1894.
15. Uhl, M., Debus, J. (2014) Chordoma: an assessment of future treatment and management strategies. Expert Opin Orphan Drugs, 1â?9.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



