Research Article - (2024) Volume 9, Issue 10
Quality of Recovery in Pediatrics After Tonsillectomy Under Total Intravenous Anesthesia Versus Sevoflurane Anesthesia
2Centro Hospitalar Universitário de Santo António, Local Health Unit of Santo António, Anesthesiology, Anesthesiology Clinic Intensive Medicine Emergency and Urgency, Anesthesiology Service, Portugal
3Department of Science and Technology, Open University, Porto, Portugal
#Equally contribution
Received Date: Sep 08, 2024 / Accepted Date: Oct 15, 2024 / Published Date: Oct 21, 2024
Copyright: Copyright: ©2024 Mafalda Lisboa, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited.
Citation: Lisboa, M., Duarte, S., Nunes, C.S., Machado, H. (2024). Quality of Recovery in Pediatrics After Tonsillectomy Under Total Intravenous Anesthesia Versus Sevoflurane Anesthesia. J Clin Rev Case Rep, 9(10), 01-10.
Abstract
Introduction: Inhalational anesthetics are often the first choice in pediatric anesthesia. However, the most recent literature demonstrates possible advantages of total intravenous anesthesia (TIVA). The goal of this study was to compare the postoperative quality in children submitted to tonsillectomy under TIVA versus sevoflurane anesthesia.
Materials and Methods: Prospective observational case-control study (Sevoflurane vs TIVA) including children submitted to (adeno) tonsillectomy to compare the quality of anesthesia considering intra and postoperative parameters. Data was collected from clinical records, anesthetic monitoring and interviews.
Results: From the 52 children included, 25% received TIVA. TIVA group had a shorter time for liquid diet reintroduction (42 minutes vs. 95 minutes) (p<0.05) and the Sevoflurane group had a lower mean blood pressure variation (p=0.027). Mean wake up time was similar for both groups (11.3±6.2 minutes for TIVA and 11.6±5.3 minutes for Sevoflurane). In PACU, TIVA group demonstrated, although not statistically significant, a shorter time of stay (40 minutes vs. 41 minutes), less emergence delirium (7.7% vs. 12.5%) and less nausea and vomiting (0% vs. 5.1%). At 24 hours, TIVA group presented, although not statistically significant, less nausea and vomiting (7.7% vs 13.5%), lower pain (69.2% with <5 on the numerical pain scale vs 56.8%) and higher parental satisfaction (10 vs 8).
Conclusion: This study suggests that TIVA for tonsillectomy may be associated with better recovery quality. However, given the limited sample size of this study, it should be repeated in a larger sample, or in a multicentric study, for more robust conclusions.
Keywords
Pediatric anesthesia, Pharmacodynamic, Bronchospasm, Bronchial aspiration, Post-anesthesia stridor, Tonsillectomy, Airway obstruction
Introduction
Pediatric anesthesia has its own specificities as the needs of infants and young children are different from those of adults. It is imperative to know the pharmacokinetic and pharmacodynamics principles in pediatric population to mitigate the risks of underdosing or toxicity. The pediatric population has an anesthetic risk significantly higher than adult surgical patients, the occurrence of anesthesia-related fatal outcomes is 10 times higher in children [1]. The estimated occurrence rate of severe critical events during the perioperative period is 5.2% and respiratory related events, such as laryngospasm, bronchospasm, bronchial aspiration, and post-anesthesia stridor are the most frequent [2].
Tonsillectomy (with or without adenoidectomy) is one of the most common surgical procedures performed in children, representing a major impact on pediatric health care. The major indications for tonsillectomy include airway obstruction, resulting in sleep-disordered breathing or obstructive sleep apnea, and recurrent infection [3]. Airway management for tonsillectomy is particularly challenging and the incidence of laryngospasm is higher than during other surgical procedures [4]. Tonsillectomy can be executed by numerous techniques, the most common are the cold tonsillectomy, monopolar cautery and coblation, using radiofrequency ablation. The first is the most traditional and is associated with less postoperative pain. Monopolar cautery uses an electrical current creating temperatures from 400 to 600ºC, achieving minimal intraoperative bleeding and reducing hemorrhage in the first 24 hours, while the coblation technique offers coagulation benefits similar to those of monopolar cautery, using lower temperatures, leading to less postoperative pain in comparison [5]. Complications associated with tonsillectomy occur with an overall frequency of 19% [6] and include anesthesiarelated side effects, such as laryngospasm and/or bronchospasm, respiratory complications (the most frequent), followed by secondary and primary hemorrhage. Other complications are dehydration, infection, burn injuries, temporomandibular joint dysfunction and velopharyngeal insufficiency. Mortality posttonsillectomy is a rare event. Tonsillectomy is associated with significant pain and postoperative nausea and vomiting (PONV) and other general issues in postoperative care include return to normal diet and activity [7].
Inhalational anesthesia using sevoflurane and total intravenous anesthesia (TIVA) with propofol are two techniques widely used to maintain anesthesia in pediatric patients undergoing general anesthesia. However, discussion about the choice of the proper anesthesia technique continues among anesthesiologists [8].
Inhalational anesthetics are very commonly used in pediatric anesthesia because they are effective, reliable, secure, easily administered, stable and without major end organ sequelae [9]. They are frequently used for both induction and anesthesia maintenance. Meanwhile, TIVA is becoming an appealing option as it is probably an effective technique to maintain general anesthesia in pediatric outpatient surgery and seems to increase parental satisfaction [8].
General anesthesia may induce anesthesia-related adverse effects, such as emergence delirium (ED), PONV, postoperative pain and short-term memory impairment. The quality of recovery seems to be affected by the anesthetic [10].
Regarding inhalational anesthesia, the mechanism of action of inhaled anesthetics is not fully understood, although a current working hypothesis is that inhaled anesthetics intensify the inhibitory activity of postsynaptic channels (gammaaminobutyric acid (GABA) and glycine) and restrain excitatory synaptic channel activity (nicotinic acetylcholine, serotonin and glutamate receptors) in the central nervous system [11]. Sevoflurane has been described as the agent of choice for mask induction in children, considering its lack of airway irritation, hemodynamic characteristics and lower pungency. Moreover, the safety and efficacy of sevoflurane are well established. In contrast, both desflurane and isoflurane are considered less suitable for anesthesia induction due to airway irritation [12,13]. Sevoflurane has the advantages of minimal airway irritation, rapid, simple and pain-free induction by mask and quick recovery from anesthesia [9,14] On the other hand, sevoflurane affects a variety of systems that can result in cardiovascular, central nervous system and respiratory side effects, such as hypotension, cardiac depression and ventilatory depression [15]. Postoperative adverse events associated with inhaled anesthetics include pain, PONV, headache, dizziness, cognitive dysfunction and ED [15].
TIVA techniques use propofol as the main drug for induction and maintenance of anesthesia. Propofol is an intravenous anesthetic, it may be administered as a bolus or an infusion, or some combination of the two. Its mechanism of action is related to the effects on GABA- mediated chloride channels in the brain, enhancing the inhibitor effects of this neurotransmissor [16].
According to recent studies, the use of TIVA seems to be associated with reduced PONV, improved quality of emergence from anesthesia and reduced ED in children. Besides that, TIVA anesthesia seems to be associated with overall reduced costs and reduced airway reactivity, laryngospasm and bronchospasm [9,17]. Furthermore, the changes in airway reactivity facilitate extubation and result in a minimal incidence of laryngospasm and stridor after extubation [18]. TIVA permits out-of-operating room procedures to be safely performed [19,20]. In contrast, the disadvantages of TIVA in children include the need for venous access, pain on injection, a higher risk of bacterial contamination, the need for specialized equipment (infusion pumps), risk of associated metabolic phenomena and potential for disconnection with risk of awareness. Topical anesthetic creams have helped minimize the discomfort of needle insertion [17,18,21]. The only absolute indication to use TIVA over inhalational maintenance for anesthesia is when there is a risk of malignant hyperthermia. There are several situations where it may be more challenging to use TIVA in pediatrics. These include neonates and young infants, obese children and children that are big for their age, due to their physiological differences [17].
Among the most common complications in the immediate postoperative period after tonsillectomy is the ED. It is common in preschool children undergoing general anesthesia and symptoms include agitation, hyperactivity with flailing movements, confusion, and failure to engage with people and the surroundings [22]. It usually begins at the start of emergence, but the onset can be as long as 45 min after the termination of anesthesia. While there are identifiable associations with the condition that relates to patient, surgical, and anesthetic factors, the underlying causation remains unknown. ED may be the consequence of other etiologies, including hypoxemia, pain, bladder distension and nausea, causes that must be excluded, as it is a diagnosis of exclusion. According to a study about ED in children, the use of propofol-remifentanil TIVA decreased the incidence of ED compared with sevoflurane anesthesia, so there may be merit in modifying the anesthesia technique in children with the highest risk [23].
The primary goal of this study is to assess the quality of postoperative recovery after anesthesia with TIVA and sevoflurane for tonsillectomy surgery in children, according to parameters such as perioperative respiratory complications, postoperative pain, ED, PONV and other postoperative outcomes.
Materials and Methods
Study Design
The study was approved by the Hospital Board and Ethics Committee. Written informed consent was collected by all legal representatives to participate in the study, and an information leaflet about the study was explained to all children and legal representatives, including the pain scales used to evaluate pain after surgery.
Observational, prospective case-control study (case: sevoflurane anesthesia, control: TIVA), including all consecutive children between 4 and 10 years old, scheduled for elective tonsillectomy/ adenotonsillectomy surgery in a University Hospital during one month.
The surgical procedure selected for this study was tonsillectomy with or without adenoidectomy, as it is a painful procedure, with a high incidence of postoperative pain, ED and PONV, allowing comparison between the two anesthetic techniques in a more similar population. The type of induction was not considered for the definition of the anesthetic technique.
No unnecessary procedures besides the ones required for surgery were performed to obtain data for this study.
Inclusion criteria included all the consecutive children proposed for tonsillectomy with or without adenoidectomy that had an American Society of Anesthesiologists (ASA) physical status of 1 or 2, between 4 and 10 years old.
Exclusion criteria included children with hypersensitivity to the used drugs, lack of parental consent for the child’s participation in the study, inability of children to understand the pain scale appropriate to their age and loss of data.
Ensuring confidentiality and anonymity, the following data were collected: Demographic data: age, sex, weight (kg), ASA physical status, co-morbidities, preoperative anxiety (evaluated by Modified Yale Preoperative Anxiety Scale (mYPAS). Surgical and anesthetic data: surgery regimen (day surgery, day surgery with overnight stay, inpatient surgery), duration of surgery, type of anesthesia, maintenance general anesthetic, duration of the anesthesia, time from end of surgery until end of anesthesia, type of induction, parents present at induction, opioids administered (drugs and doses), intraoperative analgesia administered (drugs and doses), PONV prophylaxis administered (drugs and doses), heart rate (maximum and minimum), mean blood pressure (MBP) (maximum and minimum), perioperative complications. Data related to the postoperative period: At discharge from post anesthetic care unit (PACU): Duration of stay in PACU (min), drugs administered in PACU (drugs and doses), ED (Pediatric Anesthesia Emergence Delirium (PAED) scale - observational scale), PONV (yes/no), pain at discharge from PACU and maximum pain at PACU (Faces Scale from 4 to 6 years old and Numeric Scale (NS) from 7 to 10 years old), opioids administered (drugs and doses). Data related to the postoperative period up to 24h after surgery: The legal representatives and children were interviewed by phone 24 hours after the surgery. The questionnaire included: nausea (yes/no), vomiting (yes/no), pain at 24 hours after surgery (Faces Scale from 4 to 7 years old and Numeric Scale from 7 to 10 years old), parental satisfaction (0- 10), reintroduction of liquids in the diet (hours). Postoperative data up to 3 weeks after surgery: we collected postoperative complications up to ears nose and throat examination (ENT) reevaluation appointment.
The data were collected before, during and after the surgery, resorting to clinical records, interviews with the legal representatives and anesthetic monitoring.
Data Analysis
We planned a study of independent cases and controls with 1 control(s) per case. Considering the reported incidence in the literature of ED comparing sevoflurane anesthesia with TIVA, prior data indicated that the probability of exposure among controls is 0,128, if the true odds ratio for disease in exposed subjects relative to unexposed subjects is 4,99, we needed to study 42 case patients and 42 control patients to be able to reject the null hypothesis that this odds ratio equals 1 with probability (power) 0,8. The Type I error probability associated with this test of this null hypothesis is 0,05. We used a continuity-corrected chi-squared statistic or Fisher’s exact test to evaluate this null hypothesis.
Statistical evaluation was performed using the IBM® Statistical Package for the Social Sciences (SPSS) data analysis software, version 26.
Results were obtained from the descriptive analysis of the population using the count and percentage of ordinal and cardinal categorical variables and using the mean, standard deviation (SD), median and interquartile range (IQR) of continuous variables (according to normality of data).
Parametric tests were made for the continuous variables that followed a normal distribution and non-parametric tests were made for the variables that didn’t. Chi-square test and Exact Fisher test were used to evaluate dichotomous variables. Relative risk and odds ratio were used to test the impact of the case (sevoflurane) over control (TIVA) on the evaluated outcomes, a 95% confidence interval (CI) was used.
Results
Among 66 eligible patients, 62 were included in the study and 52 were included in the data analysis. The 10 children were excluded either due to the researchers’ inability to access clinical data or because of a delay in psychomotor development compromising outcomes evaluation. An overview of the study selection process is presented in Figure 1. The study had to be terminated due to time constraints despite the number of patients included.

Figure 1: Flowchart of the study
Heart rate and time between end of surgery and anesthesia have a normal distribution, the remaining continuous variables do not (according to the Kolmogorov-Smirnov test with Lilliefors correction). However, due to the reduced sample size, non-parametric tests were applied to all continuous variables.
The demographic data are shown in Table 1. Median age was 5.0 years and most of the patients were male (53.8%). Regarding ASA physical status, 53.8% of patients had a status of 2. Most of the patients were submitted to surgery in an ambulatory regimen with overnight stay n=28 (53.8%). Considering the sevoflurane group, most patients stayed overnight n=22 (56.4%), while in the TIVA group, most children had day surgery n=7 (53.8%). TIVA technique was used in 25.0% (n=13) of patients and maintenance with sevoflurane in 75.0% (n=39). The median duration of anesthesia was 71.5 minutes. Sevoflurane group had a median time of anesthesia of 72.0 minutes and the TIVA group of 58.0 minutes. No significant differences were found between the two groups in sex ratio, age, weight, surgical regimen, duration of anesthesia and induction technique. Conversely, we found a significant difference in ASA physical status (p=0.001) and surgical technique (p=0.005), between groups. Most patients from the TIVA group had an ASA physical status of 2 n=12 (92.3%), while an ASA physical status of 1 was more common in the sevoflurane group n=23 (59.0%). The surgical technique most used in the sevoflurane group was the cold technique n=34 (87.2%), coblation was the most common in the TIVA group n=7 (53.8%). No significant differences were found between surgical technique and postoperative outcomes in our sample (p>0.05).
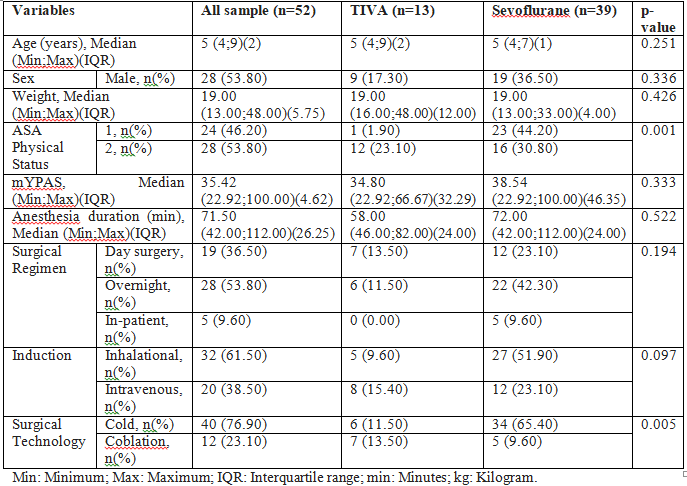
Table 1: Demographic data.
Preoperative anxiety evaluated through mYPAS showed a median score of 35.4. The median score in the TIVA group was 34.4 and in the inhalation anesthesia group was 38.5. There are no significant differences between the two groups regarding preoperative anxiety. All children participating in the study had their parent presents during induction of anesthesia.
Data related to the intraoperatively administered drugs are described in Table 2. We found a significant difference in median milligram per kilogram (mg/kg) of the intraoperative administration of tramadol (p=0.002), lidocaine (p<0.001), ketamine (p<0.001) and methylprednisolone (p=0.004). The TIVA group had a higher median dose for all drugs, except tramadol, which was higher in the sevoflurane group. We did not find any statistically significant difference in the dose per kg administration of other drugs.
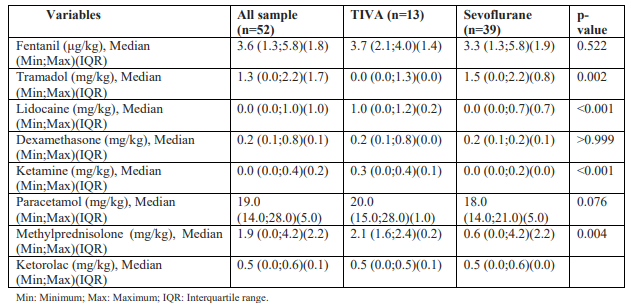
Table 2: Intraoperatively administered drugs.
Perioperative data are demonstrated in Table 3. The mean time between the end of the surgery and the end of the anesthesia was 11.5 (±5.5) minutes. Wake up time in the sevoflurane group was 11.6(±5.3) minutes and in the TIVA group was 11.3(±6.2) minutes (p=0.532). The mean heart rate variation was 34.5(±13.7) beats per minute and the median MBP variation was 21.0 mmHg. Looking at the two groups, we found that the mean heart rate variation in the TIVA group was 36.8 (±14.9) beats per minute against 33.8 (±13.4) beats per minute in the sevoflurane group. This difference was not statistically significant (p=0.732). The median MBP variation in the sevoflurane group was 18.0 mmHg and in the propofol group was 26.0 mmHg. We found a significant difference in MBP variation during anesthesia (p=0.027), being the TIVA group the one that had a greater variation. We encountered solely one intraoperative complication, it was a bleeding during the extubation period requiring bipolar coagulation and it occurred in the sevoflurane group and the cold tonsillectomy technique was performed.
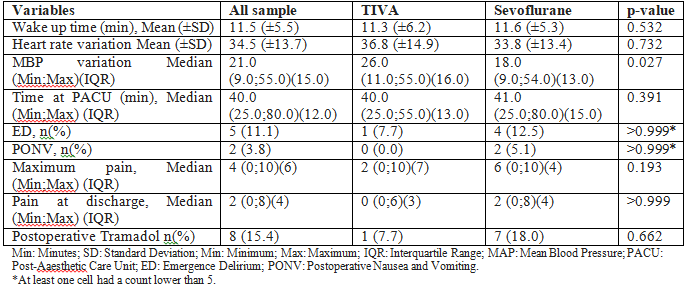
Table 3: Perioperative and PACU data
Data relative to the PACU are presented in Table 3. The median time spent in PACU was 40.0 minutes; 40.0 minutes for the propofol group, which is less than the sevoflurane group (41.0 minutes). However, this difference in time until discharge from PACU was not statistically significant (p=0.391). PONV frequency in PACU was 3.8% (n=2), both patients from the sevoflurane group. The median pain experienced at discharge from PACU was 2 (NS) and the median of maximum pain experienced was 4 (NS). Comparing the groups, median pain experienced at discharge from PACU in the sevoflurane group was 2 (NS) and in the propofol group was 0 (NS). Considering the maximum pain suffered in PACU, the median in the sevoflurane group was 6 (NS) and in the TIVA group was 2 (NS). There was no significant difference found between TIVA and sevoflurane groups regarding postoperative pain in PACU, either maximum (p=0.193) or at discharge (p>0.999). ED, assessed by PAED scale, had a global incidence of 11.1% (n=5) in our sample. Regarding type of anesthesia, in the sevoflurane group 12.5% (n=4) of children experienced ED, while in the TIVA group only 7.7% (n=1) presented ED. Administration of tramadol postsurgery was assessed and most of the tramadol administration after surgery occurred in the sevoflurane group n=7 (18.0%). We did not document any statistical difference between the two groups considering postoperative tramadol administration (p=0.662). Table 4 shows the result of the 24-hour post-surgery interview. At the 24-hour assessment, 12.0% (n=6) of the patients interviewed had PONV and 60.0% of children experienced pain at 24h below 5(NS). The PONV incidence in the sevoflurane group was 13.5% (n=5) and in TIVA group 7.7% (n=1). Regarding pain at 24 hours post-surgery, 69.2% (n=9) of children who received TIVA claimed to have pain below 5 (NS) and this was affirmed by 56.8% (n=21) of children from the sevoflurane group. However, there is no significant difference between the two groups (p=0.522). The median time of liquid diet reintroduction was 60 minutes after surgery, when comparing TIVA and sevoflurane, the TIVA group had a median time of liquid diet reintroduction of 42.0 minutes, and the sevoflurane group had a median of 95.0 minutes. The TIVA group reintroduced the liquid diet earlier, with a statistically significant difference (p=0.005) and a odds ratio (OR) of 0.191, representing an 81.0% probability of an earlier diet reintroduction with TIVA vs sevoflurane anesthesia. Concerning parental satisfaction, they reported a median satisfaction rating of 9, in the sevoflurane group the median was 8 and in the TIVA group was 10. No statistical difference regarding parental satisfaction was found (p=0.480).
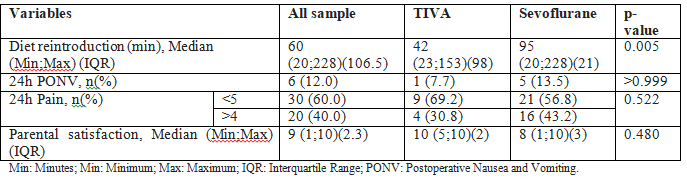
Table 4: 24 hour assessment data.
Considering postoperative data up to 3 weeks after surgery, there were two postoperative complications observed in the ENT reevaluation appointment. One of them, from the sevoflurane group, was a hospitalization 24 hours after surgery due to complete aphagia. The other episode was an emergency department visit prompted by a refusal to consume food and belonged to the TIVA group.
Discussion
Inhalation anesthesia is widely acknowledged by the majority of pediatric anesthetists as the gold standard [8]. In our study, 75% of the population had sevoflurane as the anesthetic of maintenance, which is consistent with the literature, although it is important to consider that the TIVA technique is gaining popularity, as recent studies have suggested better postoperative outcomes associated with this technique.
In our investigation, we observed that the mean wake up time was higher in the sevoflurane group, however, we did not find the difference statistically significant (p=0.532). A meta-analysis from 2022 demonstrated that pediatric patients who receive sevoflurane tend to have shorter recovery times to eye opening, being associated with shorter times of extubation [24]. In contrast, another study found no differences in extubation time and recovery time between the two techniques [25]. The rapid recovery time related to sevoflurane anesthesia can be justified by the pharmacodynamic and pharmacokinetic of sevoflurane. The recovery depends only on exhaling the anesthetic that has low blood-gas solubility, allowing a rapid washout, as its metabolism does not contribute significantly to its elimination. Nevertheless, it is crucial to take into account that the duration of anesthesia affects the time between the end of the surgery and the end of the anesthesia [11], and our sevoflurane group had an higher median duration of anesthesia compared with TIVA, what can interfere in our conclusions about wake up time.
Sevoflurane causes a decrease in blood pressure and cardiac output that is dependent on the dosage, primarily by reducing systemic vascular resistance [12]. As for propofol, it causes vasodilation by inhibiting sympathetic vasoconstrictor activity and, especially when administered as a bolus, can cause a profound reduction in the mean arterial pressure [16]. The incidence of cardiopulmonary complications in general is not significantly different when volatile anesthetics or intravenous anesthetics are used for induction and maintenance of general anesthesia [10]. Regarding hemodynamics, the results of this study showed a significant difference in the MBP variation (p=0.027), with the sevoflurane group exhibiting greater hemodynamic stability. However, this difference seems not to have significant hemodynamic impact as any patient needed pharmacologic intervention to control this effect. In heart rate variation, we found no significant difference.
The study of the postoperative period is relevant as it is crucial for the well-being of children and their parents. The literature shows distinct findings on the impact of type of anesthesia. Kocaturk et al. in 2018 found no statistical significant difference between propofol versus sevoflurane anesthesia in children between 3 and 7 years old submitted to comprehensive dental treatment [25]. In contrast, in 2020, Sheikhzade et al. evaluated the quality of recovery between TIVA and sevoflurane anesthesia in children aged between 2 and 10 years old, submitted to various surgical procedures, and demonstrated a significant difference in the time of staying in recovery, with a mean discharge time of 25 minutes for sevoflurane and 35 minutes for TIVA 10. Our findings indicate that patients who received TIVA tended to have shorter PACU stays, although no statistical difference was observed.
Postoperative pain has a significant impact on children and tonsillectomy is associated with moderate-to-severe pain. In our study, we observed that the median of maximum pain experienced and the median of pain at discharge from PACU were higher in children who received sevoflurane. However, the surgical technique can affect postoperative pain. The cold technique is associated with less postoperative pain and bleeding than coblation technique [5]. Although the TIVA group tended to have lower pain scores, the surgical technique most used on these children was coblation. No significant differences were found between surgical technique and postoperative outcomes in our study. A recent meta-analysis showed that postoperative pain in children receiving TIVA was less frequent than in the ones that received sevoflurane. This study also indicated that propofol produced an opioid-sparing effect and delayed the first request for rescue analgesia [24]. Sheikhzad et al evidenced that TIVA reduced postoperative pain [8]. These results are consistent with our findings, however, our study did not find this difference to be statistically significant. We also compared the administration of tramadol in the postoperative period and observed that the sevoflurane group received tramadol more frequently, but no statistical difference was found.
One of the most concerning outcomes of postoperative pain is pain with swallowing, because it limits the ability to eat and drink and can lead to an increased time of food reintroduction. There is limited literature that directly compares the reintroduction of fluids after TIVA and sevoflurane anesthesia. In 2005, Glaisyer et al. found that drinking occurred 24 minutes earlier in the propofol/ remifentanil group compared with inhalational anesthesia [20]. In agreement with this, our study found that children from the TIVA group reintroduced liquid diet significantly earlier, with a median time of 42 minutes in the TIVA group and 95 minutes in the sevoflurane group. We documented an 81% probability of an earlier diet reintroduction with TIVA vs sevoflurane anesthesia. As children undergoing tonsillectomy face a higher risk for PONV and subsequent dehydration, it is important to recognize the risk factors to this complication and know the measures to reduce it, as it is a common reason for hospital readmission. The risk factors are previous history of PONV, motion sickness, female sex, long duration of surgery (>30 minutes), administration of inhalation anesthetics and longer-acting opioids [26]. In fact, a study in children aged ≥ 2 and ≤ 6 years, undergoing strabismus repair surgery showed that the PONV occurrence rate in patients with sevoflurane anesthesia is 12.14%, which is markedly higher than in ones with propofol anesthesia (6.65%) [24]. Our results showed incidence of PONV only in the sevoflurane group. This can be justified by the antiemetic properties of propofol, probably because it has a depressant effect on the chemoreceptor trigger zone and vagal nuclei [16]. In order to minimize PONV, it is recommended generous hydration with crystalloids and prophylactic intravenous use of a 5-HT3 antagonist, such as ondansetron, and dexamethasone. Ondansetron prevents early PONV and dexamethasone late PONV (>6 hours) [26]. Our sample had a double anti-emesis therapy almost universal (except 1 patient), what possibly explains our low incidence of PONV.
There is no clear reason for the higher incidence of ED after inhalational anesthesia, but the rapid emergence associated with the sevoflurane anesthesia, can be one of the causes [27]. The quick emergence could be a cause by itself or could be associated with emergence before the onset of effective analgesia in the presence of surgical pain, but it is proven that this condition can occur after non-painful procedures too. Nevertheless, propofol is also associated with a rapid emergence and has a lower incidence of ED. Hence, the cause of ED in the immature nervous system is more likely attributed to the neuropharmacological properties of the agents themselves rather than a rapid emergence accompanied by delayed onset of analgesia [22]. According to Chandler et al. the use of propofol-remifentanil TIVA decreased the incidence of ED by more than half, presenting an incidence with sevoflurane of 38,30% and with TIVA of 14,90% [23]. In 2022, a meta-analysis about the incidence of ED in children also showed that it occurred less frequently with propofol anesthesia than with sevoflurane [24]. Our findings demonstrated that 12.5% of children who received sevoflurane had ED comparing to 7.7% of patients from the TIVA group. Thus, ED was more common in the sevoflurane group, but we did not find this difference statistically significant
It is essential to consider that ED can be affected by preoperative anxiety. A study about preoperative anxiety and ED showed that every 10% increase in anxiety scores causes a 10% increase in ED [28]. The study we conducted evidenced a median of preoperative anxiety of 35.4 (mYPAS) and no significant difference between sevoflurane and propofol. All children enrolled in the study had their parents present during induction, thus this could be one of the reasons for the similar results. There are some characteristics that increase the risk of both preoperative anxiety and ED, such as younger children, more emotional, more impulsive and less social. Furthermore, parental anxiety is a predictor of preoperative anxiety in children. The role of parental presence during anesthesia induction is not totally clear, but research demonstrates that a program that consists of educating parents about the techniques, enrolling them in distracting their own child in the waiting room and during anesthesia induction reduced children’s anxiety before surgery and incidence of ED, shortened discharge time after surgery and reduced analgesic consumption [28,29].
When evaluating postoperative vomiting after a pediatric adenotonsillectomy in children aged 3-16 years who were scheduled for a tonsillectomy, a study observed no significant difference between TIVA and sevoflurane maintenance during the 24-hour period thereafter. They also showed that postoperative vomiting occurred most frequently in the first 6 hours after discharge from PACU in both groups [30]. In our study, children from the sevoflurane group had a higher frequency of PONV at the 24 hour assessment, but no statistical difference was observed.
Concerning the evaluation of pain over a 24-hour period, most of children experienced pain below 5, nevertheless, the TIVA group tended to have more children claiming less pain (below 5). Despite these findings, no statistically significant difference was evidenced.
A clinical trial about recovery characteristics of propofol and sevoflurane anesthesia evidenced significantly higher parental satisfaction scores (grading their satisfaction level from 0-very dissatisfied - to 10-very satisfied) in TIVA group (median 9, and sevoflurane with 6.5 of median).27 In conformity with this study, our research demonstrated that parents of children in the TIVA group reported a median satisfaction rating of 10, whereas those in the sevoflurane group reported a median satisfaction rating of 8 (p=0.480). It is crucial to notice that postoperative complications influence parental satisfaction and the choice of surgical technique could have some implications for that.
Finally, this study still has some limitations, which should be addressed. First, the sample size is smaller than expected, which therefore limits our conclusions. Furthermore, as this study desires to compare two anesthetic techniques, it is preferred to achieve an equivalent sample size for both groups. However, this requirement is not currently met, as there is an imbalance in the number of samples between the TIVA group (n=13) and the sevoflurane group (n=39), which results from the nature of the study, as merely observational, not influencing anesthesiologits choices. There are other inherent biases in this research, as it is an observational study. The anesthetic approach, including the selection of drugs and postoperative strategies in the PACU, varied considerably, as it was determined by the attending anesthesiologists. For instance, the use of tramadol during surgery might impact the level of postoperative pain experienced, while the administration of anti-emetic drugs could affect the occurrence of PONV. The existence of two surgical techniques also introduces an additional factor that may impact the outcomes. The postoperative evaluation was essentially carried out by 2 non-blinded observers, which could affect the results due to the subjectivity of the evaluation and knowledge of the anesthetic technique applied.
Despite these limitations, this study also presents some relevant aspects. It assessed a remaning question in debate in pediatric anesthesia, with few literature evaluating the impact of anesthetic technique in the reintroduction of diet after surgery, as well as influence on immediate postoperative pain. As far as we are aware, is the first study assessing this question in our country? A future study would benefit from implementing a randomized and double-blinded design, while also ensuring a larger and more homogeneous sample size.
Conclusion
This observational study revealed that children who were anesthetized with TIVA reintroduced the liquid diet earlier when compared to children who received sevoflurane anesthesia. Moreover, anesthesia with sevoflurane was demonstrated to be more stable regarding our results in MBP variation during anesthesia. We did not find any significant difference in other outcomes, namely wake up time, postoperative pain, PONV, ED, parental satisfaction and PONV and pain 24 hours after surgery, although TIVA tended to be associated with better quality of recovery. More investigations should be performed to assess, in a clearer way, the recovery profile of TIVA and inhalation anesthesia.
References
1. Gonzalez, L. P., Pignaton, W., Kusano, P. S., Módolo, N. S., Braz, J. R., & Braz, L. G. (2012). Anesthesia-related mortality in pediatric patients: a systematic review. Clinics (Sao Paulo, Brazil), 67(4), 381–387.
2. Habre, W., Disma, N., Virag, K., Becke, K., Hansen, T. G., Jöhr, M., Leva, B., Morton, N. S., Vermeulen, P. M., Zielinska, M., Boda, K., Veyckemans, F., & APRICOT Group of the European Society of Anaesthesiology Clinical Trial Network (2017). Incidence of severe critical events in paediatric anaesthesia (APRICOT): a prospective multicentre observational study in 261 hospitals in Europe. The Lancet. Respiratory medicine, 5(5), 412–425.
3. Wald, E.R (2023). Tonsillectomy and/or adenoidectomy in children: Indications and contraindications. In: Morven S Edwards GCI, FAAP, ed. UpToDate.2023.
4. Sadhasivam, S. (2023). Anesthesia for tonsillectomy with or without adenoidectomy in children. In: UpToDate.2023.
5. Sharma, S., Andreoli, S., Josephson, G.D. (2016). Tonsillectomy and Adenoidectomy: Current Techniques and Outcomes. Int J Head Neck Surg. 2016, 7:104-108.
6. De Luca Canto, G., Pachêco-Pereira, C., Aydinoz, S., Bhattacharjee, R., Tan, H. L., Kheirandish-Gozal, L., Flores-Mir, C., & Gozal, D. (2015). Adenotonsillectomy Complications: A Meta-analysis. Pediatrics, 136(4), 702– 718.
7. Messner AH: Tonsillectomy (with or without adenoidectomy) in children: Postoperative care and complications. In: UpToDate.2023.
8. Sheikhzade, D., Razaghipour, M., Seyedhejazi, M., Aliakbari Sharabiani, B., Marahem, M. (2020). A Comparison of the Sevoflurane and Total Intravenous Anesthesia on the Quality of Recovery in 2 to 10-Year-Old Children. Iran J Pediatr, 31(1), e105900.
9. Lerman, J., & Jöhr, M. (2009). Inhalational anesthesia vs total intravenous anesthesia (TIVA) for pediatric anesthesia. Paediatric anaesthesia, 19(5), 521–534.
10. Scheiermann, P., Herzog, F., Siebenhofer, A., Strametz, R., & Weberschock, T. (2018). Intravenous versus inhalational anesthesia for pediatric inpatient surgery - A systematic review and meta-analysis. Journal of clinical anesthesia, 49, 19-25.
11. Campagna, J.A., Miller, K.W., Forman, S.A. (2003). Mechanisms of actions of inhaled anesthetics. N Engl J Med, 348, 2110-2124.
12. De Hert, S., & Moerman, A. (2015). Sevoflurane. F1000Research, 4(F1000 Faculty Rev), 626.
13. Olsson G. L. (1995). Inhalational anaesthesia at the extremes of age: paediatric anaesthesia. Anaesthesia, 50 Suppl, 34–36.
14. Brioni, J. D., Varughese, S., Ahmed, R., & Bein, B. (2017). A clinical review of inhalation anesthesia with sevoflurane: from early research to emerging topics. Journal of anesthesia, 31(5), 764–778. 15. Patel, S. S., & Goa, K. L. (1996). Sevoflurane. A review of its pharmacodynamic and pharmacokinetic properties and its clinical use in general anaesthesia. Drugs, 51(4), 658– 700.
16. Folino, T.B., Muco, E., Safadi, A.O., Parks, L.J. (2023). Propofol. In. StatPearls, Treasure Island (FL): StatPearls Publishing Copyright; 2023.
17. Anderson, B. J., & Bagshaw, O. (2019). Practicalities of Total Intravenous Anesthesia and Target-controlled Infusion in Children. Anesthesiology, 131(1), 164–185.
18. Gaynor, J., Ansermino, J.M. (2016). Paediatric total intravenous anaesthesia. BJA Education, 16, 369-373.
19. Malherbe, S., Whyte, S., Singh, P., Amari, E., King, A., & Ansermino, J. M. (2010). Total intravenous anesthesia and spontaneous respiration for airway endoscopy in children- -a prospective evaluation. Paediatric anaesthesia, 20(5), 434–438.
20. Glaisyer, H. R., & Sury, M. R. J. (2005). Recovery after anesthesia for short pediatric oncology procedures: propofol and remifentanil compared with propofol, nitrous oxide, and sevoflurane. Anesthesia and analgesia, 100(4), 959–963.
21. Jalota, L., Kalira, V., George, E., Shi, Y. Y., Hornuss, C., Radke, O., Pace, N. L., Apfel, C. C., & Perioperative Clinical Research Core (2011). Prevention of pain on injection of propofol: systematic review and meta-analysis. BMJ (Clinical research ed.), 342, d1110.
22. Nair, S., & Wolf, A. (2018). Emergence delirium after paediatric anaesthesia: new strategies in avoidance and treatment. BJA education, 18(1), 30–33.
23. Chandler, J. R., Myers, D., Mehta, D., Whyte, E., Groberman, M. K., Montgomery, C. J., & Ansermino, J. M. (2013). Emergence delirium in children: a randomized trial to compare total intravenous anesthesia with propofol and remifentanil to inhalational sevoflurane anesthesia. Paediatric anaesthesia, 23(4), 309–315.
24. Zhao, Y., Qin, F., Liu, Y., Dai, Y., & Cen, X. (2022). The Safety of Propofol Versus Sevoflurane for General Anesthesia in Children: A Meta-Analysis of Randomized Controlled Trials. Frontiers in surgery, 9, 924647.
25. Kocaturk, O., & Keles, S. (2018). Recovery characteristics of total intravenous anesthesia with propofol versus sevoflurane anesthesia: a prospective randomized clinical trial. Journal of pain research, 11, 1289–1295.
26. Zalan, J., Vaccani, J. P., & Murto, K. T. (2020). Paediatric adenotonsillectomy, part 2: considerations for anaesthesia. BJA education, 20(6), 193–200.
27. Kanaya, A., Kuratani, N., Satoh, D., & Kurosawa, S. (2014). Lower incidence of emergence agitation in children after propofol anesthesia compared with sevoflurane: a meta-analysis of randomized controlled trials. Journal of anesthesia, 28(1), 4–11.
28. Kain, Z. N., Caldwell-Andrews, A. A., Maranets, I., McClain, B., Gaal, D., Mayes, L. C., Feng, R., & Zhang, H. (2004). Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesthesia and analgesia, 99(6), 1648–1654.
29. Kain, Z. N., Caldwell-Andrews, A. A., Mayes, L. C., Weinberg, M. E., Wang, S. M., MacLaren, J. E., & Blount, R. L. (2007). Family-centered preparation for surgery improves perioperative outcomes in children: a randomized controlled trial. Anesthesiology, 106(1), 65–74.
30. Chung, J. H., Kim, Y. H., Ko, Y. K., Lee, S. Y., Nam, Y. T., & Yoon, S. H. (2010). Vomiting after a pediatric adenotonsillectomy: comparison between propofol induced sevoflurane-nitrous oxide maintained anesthesia and TIVA with propofol-remifentanil. Korean journal of anesthesiology, 59(3), 185–189.



