Case Report - (2023) Volume 8, Issue 6
Pseudosubarachnoid Hemorrhage: a Diagnostic Challenge in Some Patients who Underwent Cardiopulmonary Resuscitation
2Department of Neurology, Milad General hospital, Tehran, Iran
Received Date: May 17, 2023 / Accepted Date: May 26, 2023 / Published Date: Jun 05, 2023
Abstract
Subarachnoid hemorrhage is a serious and life-threatening condition that requires immediate diagnosis and treatment. Brain CT scan is considered one of the important diagnostic tools for this condition and requires subsequent diagnostic and therapeutic measures. But CT scan findings are sometimes deceptive and may mimic subarachnoid hemorrhage rather than true hemorrhage. Here we introduce one such condition and explain how to differentiate it from true bleeding.
Keywords
Cardiorespiratory arrest, Brain death, Cardiopulmonary resuscitation, Neurological signs
Introduction
In cases of acute and rapid loss of consciousness and coma, it is not always easy to diagnose the cause. A series of laboratory tests and imaging should be done quickly and appropriate treatment should be prescribed based on the diagnosis obtained. Cardiorespiratory arrest and the state of brain death after that is an event that happens in emergency departments and doctors try to diagnose and, if possible, perform the necessary treatment in addition to maintaining vital signs and stabilizing the patient’s heart and lung condition. Even if there is no treatment to restore the consciousness of a brain-dead patient, the diagnosis of the patient is important from a legal point of view, especially when the patient is young and does not have a history of cardiovascular diseases or has not been severely beaten. Brain imaging is a rapid and valuable diagnostic method in such emergency situations and can rule out many serious causes of brain death associated with primary brain disorders. Brain CT scan findings should be interpreted on a clinical basis. There are reports of SAH after cardiopulmonary resuscitation, but there are also cases of pseudo-SAH that may lead to misdiagnosis [1]. The prevalence of this finding in brain CT scan of brain death patients after cardiopulmonary resuscitation has been reported from 8 to 20% [2,3]. In this report, we present a case of such patients.
Case Report
The patient was a 38-year-old man who was brought to the hospital emergency room due to nausea, vomiting and confusion. The patient’s symptoms developed and progressed within a few hours. In clinical examination, the patient is sleepy and does not cooperate in giving history and examination. He had no fever and neck stiffness. There are no focal neurological signs. Pupils were meiotic and responsive to light. Fundoscopy did not show any abnormal findings. CT scan of the brain on the first day of visit did not show any bleeding or space-occupying lesion and no signs of trauma in the skull or brain tissue (Figure 1,a). Blood metabolic and toxicology tests were sent from blood and urine samples. The patient lost more consciousness and went into cardiorespiratory arrest, which was immediately followed by tracheal intubation and cardiopulmonary resuscitation. After stabilizing the cardiorespiratory condition, the patient’s consciousness dropped sharply, and the CT scan of the brain showed diffuse cerebral oedema, with hyperattenuated cisterns and cerebral sulci, compatible with diffuse SAH (Figure 1,b). Angiography of cerebral arteries did not show aneurysm or other vascular lesions. The composition of cerebrospinal fluid was normal and its color was not xanthochrome. The results of blood tests showed abnormalities in liver, kidney and blood tests, and high levels of narcotics and psychotropic drugs were reported (Tables 1 and 2).
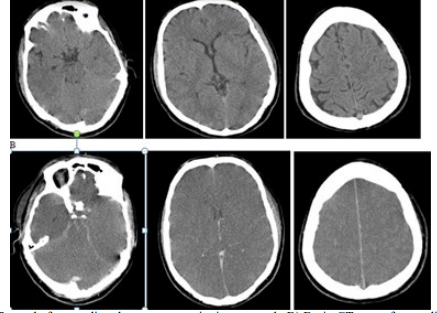
Figure 1: A) Brain CT scan before cardiopulmonary resuscitation, normal. B) Brain CT scan after cardiopulmonary resuscitation, sever brain edema and diffuse sulci effacement and obliterated basal cisterns which strongly suggests the diagnosis of SAH.
| Parameter | Value |
|---|---|
| Protein (mg/dl) | 22 |
| Glucose (mg/dl) | 65 |
| RBC | 250 |
| WBC | 0 |
| CSF color (Before CFU) | colorless-clear |
| CSF color (After CFU) | colorless-clear |
Table 1: CSF analysis and culture laboratory tests.
| Substance | Result |
|---|---|
| Tramadol | neg |
| Morphine | pos |
| Marijuana | neg |
| Tricyclic antidepressants | neg |
| Amphetamine | neg |
| Buprenorphine | pos |
| Methadone | neg |
| Benzodiazepines | neg |
| Methylenedioxymethamphetamine | neg |
Table 2: Serum toxicology study results
Discussion
Due to the availability of CT scan in most hospitals and emergency departments and the acceptable sensitivity of CT scan to show blood in the first hours and days of SAH, this method is usually used to rule out the diagnosis.The diagnosis of SAH is made when a non-contrast brain CT scan shows that a dense substance has filled the subarachnoid space. This finding is usually more prominent around the circle of Willis, as most berry aneurysms are located in this area (~65%) or in the Sylvian fissure (~30%). It should be noted that increased apparent density in the subarachnoid space is not pathognomonic of SAH. Other diagnostic possibilities include: pseudo-SAH, laminar cortical necrosis that affects the cerebral cortex not the cisterns, bacterial meningitis, tuberculous meningitis, granulomatous meningitis, neurosarcoidosis, etc. Possible mechanism in these cases is breakdown of the blood-brain barrier allowing mildly hyperdense proteinaceous material to leak into the subarachnoid space [4].
Common mechanism in almost all cases is cerebral oedema where there is a decrease in brain parenchymal attenuation and engorgement and dilatation of the superficial venous system due to an increased intracranial pressure [5,2] which is seen in hypoxic-ischaemic brain injury and recent failed cardiopulmonary arrest resuscitation.
Pseudo-SAH is a condition in which the CT scan images of the brain shows diffuse sulci effacement and obliterated basal cisterns which strongly suggests the diagnosis of SAH, but not in the autopsy, nor in the examination of the cerebrospinal fluid and the cerebral angiography [2]. This situation is seen in acute and serious situations and especially after failed cardiopulmonary resuscitation that leads to brain death.
Given and colleagues reported seven cases of generalized cerebral edema with increased attenuation of the basal cisterns, all of which were free of SAH at lumbar puncture or autopsy [5]. Also, it has been shown in the studies that pseudo-SAH in brain CT is one of the poorest prognostic criteria [2,3].
The following points should be noted regarding the findings of the CT scan that differentiates the two conditions. The amount of blood attenuation in head CT in a healthy person with a normal haematocrit of 45% is about HU 42 [6]. In true SAH, blood that has leaked from the vessels into the subarachnoid space has a higher attenuation value due to plasma absorption, with higher attenuation values between 60 and 70 HU. However, in pseudoSAH, where blood has not entered this space, attenuation values in the basal cisterns will be between 30 and 40 HU (normal limits), indicating that the vessels are dilated rather than torn, as is seen in true SAH [7]. These lower attenuation values, in association with signs of diffuse cerebral oedema, should be considered in differentiating pseudo-SAH from true SAH. Awareness of the imaging features of pseudo-SAH will help prevent over-examination of critically ill patients with possible SAH.
References
1. Opeskin, K., Silberstein, M. (2012) False positive diagnosis of SAH on computed tomography scan. J Clin Neurosci, 5 (4), 382-386.
2. Yuzawa, H., Higano, S., Mugikura, S., Umetsu, A., Murata, T., et al. (2008) Pseudo-SAH found in patients with postresuscitation encephalopathy: characteristics of CT findings and clinical importance. AJNR Am J Neuroradiol, 29 (8), 1544-1549.
3. Lee, B.K., Kim, Y.J., Ryoo, S.M., Kim, S.J., Lee, D.H., et al. (2017) Pseudo-SAH sign on early brain computed tomography in out-of-hospital cardiac arrest survivors receiving targeted temperature management. J Crit Care, 40, 36-40.
4. Mendelsohn, D.B., Moss M.L., Chason, D.P., Muphree, S., Casey, S. (1994) Acute purulent leptomeningitis mimicking SAH on ct. J Computer Assisted Tomography, 18(1), 126- 128.
5. Given, C.A., Burdette, J.H., Elster, A.D., Williams, D.W. (2003) Pseudo-SAH: A potential imaging pitfall associated with diffuse cerebral edema. American J Neuroradio, 24(2), 254-256.
6. New, P.F., Aronow, S. (1976) Attenuation measurements of whole blood and blood fractions in computed tomography. Radiology, 121(3 Pt 1), 635-640.
7. Fujita, S. (1985) Computed tomographic grading with Hounsfield number related to delayed vasospasm in cases of ruptured cerebral aneurysm. Neurosurgery, 17, 609-612.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



