Case Report - (2022) Volume 7, Issue 12
Primary intraosseous odontogenic carcinoma of the mandible: A rare presentation
Received Date: Dec 21, 2022 / Accepted Date: Dec 29, 2022 / Published Date: Dec 31, 2022
Abstract
Primary intraosseous odontogenic carcinomas (PIOC) are extremely rare tumors, developing from the residual odontogenic epithelial cells. These tumors touch the maxilla without initial damage to the oral mucosa. We report the case of a 70-year-old patient diagnosed with mandible PIOC treated with radiation and concomitant chemotherapy.
Keywords
Primary intraosseous odontogenic carcinoma, Mandible, Surgery, Radiotherapy.
Case Presentation
This is a 70-year-old patient with a left jugular mass with aphthous ulcers that have been developing for a year and a half. An otolaryngologist saw the patient. The clinical examination showed a huge mass of the left mandibular region of about 8 cm, fixed hard and painless, associated with a 3 cm left fixed lymphadenopathy. The skin and buccal mucosa next to it is normal.
A scan of the facial mass showed a tumor process centered on the mandibular symphysis, with irregular contour, tissue density with necrosis zones measuring 45*58*43 mm. This lysis process takes away the medial part of the mandibular bodies more marked on the left, with flooding of the oral floor. It is associated with multiple cervical lymphadenopathy of chains Ib and III on the left (Figure 1).
A bone biopsy showed primary intraosseous odontogenic carcinoma.
The surgery could not be performed given the local extension of the tumor and the patient received external arctherapy radiation at 70 Gy, 2 Gy per fraction, with concomitant chemotherapy with cisplatin at 40 mg/m2/week (Figure 2). The treatment passed without incident. The patient is in good clinical and radiological control with a follow-up of 12 months.
Discussion
Described for the first time by Loos in 1913 [1], PIOC is an exceptional form of epidermoid carcinoma whose point of initial involvement is bone within connection with the oral mucosa. These tumors account for 1-2% of all oral cancer.
PIOC is more common in men with a median age of 50 years [2,3].
The revealing symptoms are dominated by swelling of the jug with endooral pain. These tumors are characterized by local aggression with invasion of nearby structures. Distant metastases are rare. This atypical symptomatology with the bone starting point can mislead the diagnosis towards an infectious origin.
The CT with study of the bone windows is the gold standard. The most found radiological image is that of a poorly limited osteolytic gap or lesion, the scanner also makes it possible to highlight the uni or multifocal character of the tumor with invasion and extension towards the neighboring organs. The odontogenic cyst poses a problem of differential diagnosis, especially if the tumoral process presents well limited border [4]. An incisional biopsy is required to complete and confirm the diagnosis.
Surgical resection is the treatment of choice [7,8]. Negative margins of resection are associated with low risk of local relapse. The risk of lymph node invasion varies from 12 (7) to 70% (9) of cases. This impairment is a factor of poor prognosis according to Wenguang et al. [9]. Therefore, lymph node removal seems appropriate during the surgical procedure.
Post-operative radiotherapy showed a benefit in overall survival and in relapse-free survival. Chen et al in China concluded that postoperative radiotherapy should be given to patients with positive operative margins, tumor involvement of adjacent soft tissues, metastatic neck nodes, and partial excision of the primary tumor [10].
In case of non-resectable tumor due to tumor size or invading surrounding organs, exclusive radiation with concomitant chemotherapy can be discussed.
PIOC has a poor prognosis, with a risk of lymph node and systemic metastases. Several studies reported a 2-year survival rate of 60 to 70%, while the 5-year survival rate ranged from 30 to 40% [5,6].
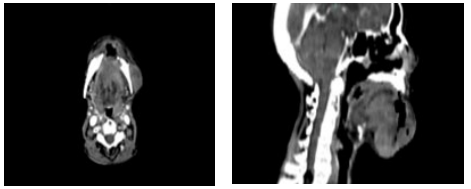
Figure 1: Facial scan in axial and sagittal section showing the tumor process.
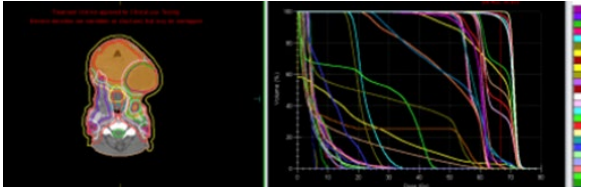
Figure 2: Trget volume and dose volume histogram
Conclusion
Primary intraosseous odontogenic carcinoma is a rare pathology that can easily be mistaken for an infected odontogenic cyst. The diagnosis is mainly based on a combination of clinical-radiological and histological arguments. With such a poor prognosis, treatment must be aggressive and multimodal.
References
1. Huang JW, Luo HY, Li Q, Li TJ (2009) Primary intraosseous squamous cell carcinoma of the jaws clinicopathologic presentation and prognostic factors. Arch Pathol Lab Med 133:1834-1840.
2. Thomas G, Pandey M, Mathew A, Abraham EK, Francis A, et al. (2001) Primary intraosseou carcinoma of the jaw: pooled analysis of world literature and report of two new cases. Int J Oral Maxillofac Surg 30:349-355.
3. Zwetyenga N, Pinsolle J, Rivel J, Majoufre-Lefebvre C, Faucher A, et al. (2001) Primary intraosseous carcinoma of the jaws. Arch Otolaryngol Head Neck Surg 127:794-797.
4. Iida S, Fukuda Y, Ueda T, Aikawa T, Arizpe JE, et al. (2006) Calcifying odon togenic cyst: radiologic fndings in 11 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101(3):356-362.
5. Huang J, Luo H, Li Q, Li T (2009) Primary intraosseous squamous cell carcinoma of the jaws: clinicopathologic presentation and prognostic factors. Arch Pathol Lab Med 133(11):1834-18340.
6. Naruse T, Yanamoto S, Sakamoto Y, Ikeda T, Yamada S, et al. (2016) Clinicopathological study of primary intraosseous squamous cell carcinoma of the jaw and a review of the literature. J Oral Maxillofac Surg 74(12):2420-2427.
7. de Morais EF, Carlan LM, de Farias Morais HG, Pinheiro JC, Martins HDD, et al. (2020) Primary intraosseous squamous cell carcinoma involving the jaw bones: a systematic review and update. Head Neck Pathol 15:608-616.
8. Lugakingira M, Pytynia K, Kolokythas A, Miloro M (2010) Primary intraosseous carcinoma of the mandible: case report and review of the literature. J Oral Maxillofac Surg 68(10):2623-2629.
9. Wenguang X, Hao S, Xiaofeng Q, Zhiyong W, Yufeng W, et al. (2016) Prognostic factors of primary intraosseous squamous cell carci noma (PIOSCC): a retrospective review. PLoS One 11 (4):e0153646.
10. Chen B, Gao L, Xu GZ (2007) Postoperative radiotherapy for primary intraosseous carcinoma of the jaws. Zhonghua Zhong Liu Za Zhi 29 (7):540-544.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



