Research Article - (2023) Volume 8, Issue 9
Medication Administration Errors for Patients Admitted at Jakaya Kikwete Car-diac Institute Dar Es Salaam Tanzania
Received Date: Aug 08, 2023 / Accepted Date: Sep 01, 2023 / Published Date: Sep 20, 2023
Copyright: ©2023 Adam Ndamayape, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited.
Citation: Ndamayape, A., Pallangyo, P., Kilindimo, S., Majani, N., Malya, R., et al. (2023). Medication Administration Errors for Patients Admitted at Jakaya Kikwete Cardiac Institute Dar Es Salaam Tanzania. J Clin Rev Case Rep, 8(9), 222-229
Abstract
Background: medication administration errors are among the most common type in medication error. They are the most common health threatening mistakes that affect the health and safety of the patient. Such mistakes are considered as a global problem which increases mortality rates, length of hospital stays, and other related costs. Objective: To explore the types, causes and why medication administration errors are not reported.
Methods: The present descriptive cross-sectional study was conducted on 75 nurses randomly selected from Jakaya Kikwete Cardiac Institute working in wards and intensive care units. A four-part questionnaire was used. The first part was on the participant demographic characteristics. The second part consisted of 15 questions on why medication errors occur. The third part consisted of 8 items asking on why medication errors are not reported and the fourth part comprised of 9 items on estimated percent of each type of error reported. Data were analysed using SPSS software version 20. The significant p-value was considered less than 0.05.
Results: Majority of the participants were female 72%, male 28%. The mean age was 34.5+-1.93, the majority had diploma level 65.4%, bachelor degree 29.3%, and master degree 5.3%. The most reported error was wrong time of administration and omission error. The most possible cause of error was tiredness due to excess work, few numbers of nurses to patient’s ratio, and heavy workload in the ward. The most reasons why medication errors are not reported was absence of incident report book for medication error, lack of protocol or guideline for medication error and fear of the staff from being fired after reporting drug error.
Conclusion: Since many medication errors are not reported by nurses, nursing leader must show positive response to nurses who are reporting medication error in order to improve patient safety. It is also very important to increase the number of qualified staffs in each working shift since heavy workload, fatigue and inadequate staff in each working shift are the most effective factor causing medication error.
Keywords
Medication administration error, Prevalence, Estimated percent, Risk factors, Cardiac institute
Introduction
Medication administration errors are a critical patient safety issue. They are universal problems contributing to patient harm in respect that quality patient care is a priority in all healthcare systems; however, patient safety can be compromised leading to potential medical harms; medication administration errors are reported to be a type of error leading to the highest rates of mortality and morbidity in patients among other medication errors [51,3-5]. Medication errors are the consequence of multiple actions of a whole chain of organizational and humans’ interactions in which the individual does not have the intention of doing wrong. Such errors may or may not lead to an adverse event, which is the actual harm that occurs to the patient [1,2]. Adverse events may also come from complications not associated with medication errors. These two groups overlap to varying degrees, and this overlap highlights the potential preventable number of adverse events.
Medical errors affected from 26.8 to 58% of the patients, including one-third from medication errors alone and may contribute to mortality [6-15]. Understanding medical errors is complex and involves country (or health care system), hospital, group and individual levels. These multi-level systems explain the low visibility of the cause-to-effect relationship between the error and its consequences and jeopardize prevention. Medication errors are major issues in the health care setting and are one of the most common types of medical errors. Medication errors can occur during prescribing; dispensing and administration of medications, and in primary, secondary and tertiary care settings [26,28]. The underlying cause for such errors may be professional practice, health care products, procedures and systems [35-41].
Although medication errors of all sorts are well investigated throughout much of the developed world, in developing nations including the case is different very few have researched [16-25].
However medication administration errors are often used as indicator of patient safety in the hospital because of their common occurrence and potential risk to patients. [31-34,50]. This area is relatively under-researched and there remain several unanswered questions. We do not know enough about how patients make attributions of adverse effects of medications, what causes the drug errors and how many errors occur. Little work has been carried out to develop and evaluate ways that will help to minimize the burden.
The purpose of this study was to explore the types, reasons why medication errors are not reported and factors effective for medication administration errors at Jakaya Kikwete Cardiac Institute
Materials and Methods
In this descriptive cross-sectional study, 75 nurses who work in different wards and intensive care units at Jakaya Kikwete Cardiac Institute from December 2022 to march 2023 were randomly selected. The inclusion criteria were physical and mental status, having at least one year of working experience with at least diploma in nursing and willingness to participate. The permission and other protocol were approved by the Jakaya Kikwete Cardiac Institute. The objectives of the study were explained to the participants and reassured confidentiality on the collected information. The data collection tool was selfmade questionnaire prepared using deferent resources related to medication administration error. It included Likert scale style, it was adjusted based on literature review [42-44]. The questionnaire was sent to the institution review board for research for content validity, the review board replied and corrections were made according to their comments then the final tool was obtained. The questionnaire was assessed using Cronbach’s alpha (r=0.806) to measure internal consistency (the higher Cronbach’s alpha, the more consistency between inter items of the questionnaire). The questionnaire consisted of four sections, the first part asked for demographic information such as age, sex, educational level, working experience and working ward. The second part asked for reasons why medication administration errors occur (15 items including: the names of many medications are similar, different medications look alike, the packaging of many medications are similar, physician medication orders are not legible, physician medication orders are not clear, physician change orders frequently, poor communication between nurses and physician, pharmacy delivers incorrect dose to the wards, pharmacy does not prepare medications correctly, pharmacy does not label medication correctly, heavy work load in the ward, inadequate staff in each working shift, tiredness due to excessive overtime work, illegible handwriting of the physician during prescription and dose omission), the third part asked for reasons why medication errors are not reported (8 items in including: Nurses do not agree with hospital definition of medication error, nurses do not recognize error occurred, filling out an incident report for a medication error takes too much time, there is no protocol for medication error, nurses believe that other nurses will think they are incompetent if they make medication error, nurses could be blamed if something happens to the patient as a result of medication error, the patient family might develop negative attitude towards the nurse or may sue the nurse if a medication error is reported, staffs are afraid of being fired after reporting medication error) and the fourth part asked for percent of each type of error reported (9 items including: wrong route of administration, wrong time of administration, wrong patient, wrong dose, expired drug, wrong dose calculation, dose omission, mislabeling and extra dose). The participants were asked to answer in Likert scale rating: Strongly disagree, disagree, neutral, agree and strongly agree with 1 to 5 value respectively. The questionnaire was distributed to nurses after obtaining their consent and collected within 24 hrs. The SPSS (v 20) was used for data analysis through descriptive statistics and spearman for correlation. Significant level of statistical differences was considered at 0.05.
Results
In this study, the majority of the participants were female (72%), the mean age was 34.5+-1.93, the majority had diploma level (65.4%), bachelor degree (29.3%), and master degree (5.3%). About 57.3% are working in ICUs, 17.3% in CCU, 18.7 in PICU and 21.3% in CT ICU. However about 53.3% nurses have 1-5 years of working experience (see Table 1). The Scoring range of the Likert scale of the study is described in table 2.
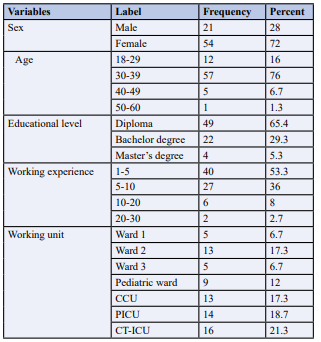
Table 1: Demographic Information.
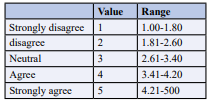
Table 2: Scoring Range of the Likert Scale of the Study [42,43,44,45].
The results totally shown that heavy workload in the ward, inadequate staffs in each working shift, tiredness due to excessive overtime are the most effective factors for occurrence of medication error (Table 3). In the prescription factor from physician point of view, factors such as illegibility of handwriting, illegibility of physician orders, dose omission and frequency change of orders from physician were pointed out as effective factors in the medication error occurrences. Great number of nurses reported that different medication looks alike and this included: furosemide looks like dexamethasone, velapamir tabs and hydralazine tabs, atropine and adrenaline, Aldactone tabs and aspirin tabs, furosemide and diazepam, gentamycin ampules and furosemide ampules and x-pen and ceftriaxone. Poor communication between nurses and physician, names of many medications are similar, many medications have similar packaging, pharmacy delivers incorrect dose in the units, pharmacy does not label medication correctly, as well as pharmacy does not prepare medication correctly were the least factor leading to medication error (Table 3) 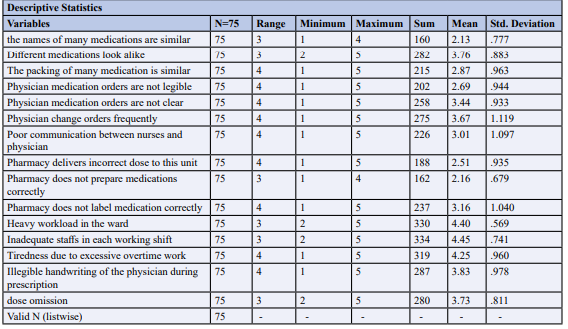
Table 3: Why medication administration error occurs.
Most of the participants agreed that there is no incident report book for medication error with mean score of 3.63. We also found that there is no protocol for medication errors in each of the unit with mean score of 4.07. Most of the nurses believe that other nurses will think they are incompetent if they make medication error that is why they do not report medication errors when happen the mean score is 4.17. The mean score about how the relative will think (their attitude towards the nurse) about the nurses in case they report the medication errors is 4.20 which means will be blamed by the patient or family related to the sick one when they report the error. Majority of the nurses agree that staffs are afraid of being fired after reporting medication error with mean score of 4.08 and that why they do not report (Table 4).
Hospital definition about medication errors and error recognition in the unit are the least reasons as to why drug errors are not reported (Table 4).
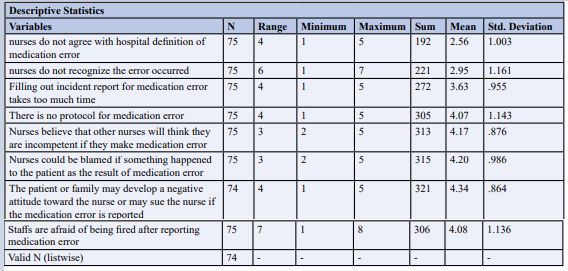
Table 4: Why Medication Errors are not Reported.
According to the findings of this study the most common types of medication error were wrong time of administration (41% to 50%) and dose omission (31% to 40%). The most possible cause was tiredness due to excess work, few numbers of nurses to patient’s ratio, heavy workload in the ward and unavailability of the drug. Another type of error reported was wrong dose (21% to 30%), in this type of error for example on infusion rate like adrenaline infusion, the chart shows only the number of mls running but no dose range, it is very likely for the nurse or doctor to come and increase or decrease the dose and no one will notice because the chart does not show the dose range and this made us conclude that there is infusion rate error though it is underestimated and overlooked. We also assessed how many percent estimate of expired drugs is administered due to various reasons and we found over 21% to 30% are given. Example of the drugs that are sometimes administered because of their unavailability by the time they are needed includes nitroglycerine, and vasopressin. Wrong dose calculation in another source of error in the hospital and accounted 31% to 40%. Dose omission estimated to range from 31 to 40% to cause medication administration errors and the other errors was extra dose.Wrong route of administration and wrong patient are least type of error reported and was estimated only between 0 to 20% (see Table 5).
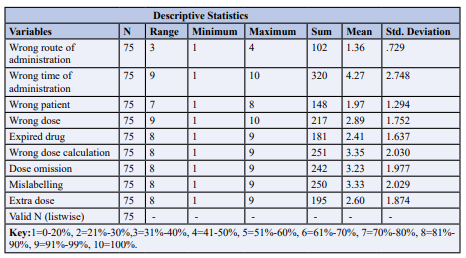
Tables 5: Estimated Percent of each type of Errors.
Discussion
This study explored the factors influencing medication administration errors, reasons why they are not reported and percent estimate of errors reported. 75 nurses working in the wards and intensive care units were recruited during the study. Heavy work load was among the most effective factors for medication errors in this paper. Eslamian et al, in their study shown that the shortage in nursing work force and consequently high workload and overtime working of nurses are common reasons for making errors [22]. Inadequate staff in each working shift was another most contributing factor for medication administration errors. Cramer H et al suggested that high workloads, low staffing, and physical or mental fatigue as the three leading causes of drug errors [51]. Tiredness due to excess overtime is another factor for occurrence of MAEs explored in this paper. However, Akram S on the study on factors effective on medication errors: A nursing view referred tiredness as factor leading to medication errors [46].
Illegible handwriting from physician during prescription, dose omission and physician medication orders not being clear are the potential causes of medication administration errors. Furthermore, nurses agreed that physicians change orders frequently and more often when they change the drug, on the medication chart is not indicated when started and sometimes when changed nurses are not informed. Most of the nurses do neither agree nor disagree that there is poor communication between them and physician. In the study on effective factors for medication errors by Shahrokhi, et al. the eligibility of physician orders, frequency change of physician orders and eligibility of handwriting of physician are contributing factors for medication errors [46,47]. Tang et al. in the study on Nurses relate the contributing factors involved in medication errors also shown the same view that eligibility of physician handwriting and eligibility of physician orders are contributing factors to the occurrence of MAEs [29].
Most of the participants do not agree that pharmacy unit delivers incorrect dose in their respective unit as well preparation of medications. Since most of the medication are prepared by nurses and few that are prepared by pharmacy unit shown relatively less error especially syrups in which there is error in dose calculation. Pharmacy sometimes do not label medication correctly when delivering to the wards.
Other factors such as drug names and label similarities, similar packaging (pantoprazole and ceftriaxone) and how different medications look alike (furosemide looks like dexamethasone, velapamir tabs and hydralazine tabs, atropine and adrenaline, Aldactone tabs and aspirin tabs, furosemide and diazepam, gentamycin ampules and furosemide ampules and x-pen and ceftriaxone) were also pointed out as factors influencing medication administration errors in this research. Sadly this factors are sometimes ignored as factors effective for medication errors but yet they are still potential causes of errors, these factors of course are not in clinical control team since they touch the manufacturers of the respective drugs. However, we can make good arrangement of the specific drugs in the treatment area or rooms but also arrange well in the shelves by separating each medicine with proper labelling so we don’t confuse them and ultimately prevent MAEs. Shahrokhi, et al on Effective factors on medication errors shown these factors to be associated with medications errors [27,46].
Regarding on why medication administration errors are not reported. Nurses shown neutrality on hospital definition about medication errors since there is no clear hospital definition well known to everyone. Again, the majority of the participants do neither agree nor disagree that errors are not recognized when they happen, sometimes errors are late recognized. Most of the participants agreed that there is no incident report for medication to record just in case error happens. There is also no protocol or hospital guideline for medication errors. Poorolajal et al concluded that lack of effective medical error reporting system is effective factors why medication errors are not reported [49]. However most of the nurses believe that other nurses will think they are incompetent if they make medication error that is why they do not report medication errors when happen. It is strongly agreed from the study that if nurses report medication errors they may be blamed by relatives. Majority of the nurses agree that staffs are afraid of being fired after reporting medication errors. Karen M et al. in their study reported that fear from the staff s after reporting is the driving force as to why they don’t report medication error. Jalal P et al. states that the fear of legal consequences was 44.4%, this fear may be due to adverse consequences such as a malpractice lawsuit, losing patient’s trust, and emotional reaction from patient and their relatives or losing occupational position/losing job [48,49].
wrong time of administration (41%-50%). Shitu et al among the types of medication errors identified in their study, wrong time error was the most prevalent [47]. Another medication error was wrong dose which was estimated between 21% -30%. Rahinu et al. studied about medication errors and adverse drug events in paediatrics inpatients shown that the most frequent errors were wrong dose 28% followed by route of administration [30]. Wrong route of administration and wrong patient errors was only 0-20% means that these types of errors occur rarely in the hospital. We also assessed how many percent estimate of expired drugs is administered and we found that about 21% to 30% occur. Wrong dose calculation is another source of error in the hospital and accounted 31% to 40%. Dose omission was estimated to range from 31 to 40% to cause medication administration errors and the other possible cause of errors was extra dose (21%-30%). Other studies reported omission error with high prevalence. The study by Acheampong et al shown high prevalence of omission error in their findings [35,47]. The possible cause of omission error in our study was due to lack of documentation of the medication chart or treatment sheet from changing one shift to another, another possible cause is unavailability of the medicine at the time prescribed by the physician.
Conclusion and Recommendation
When medication errors are not reported, the possibility of avoiding future possible preventable errors is highly minimized. This will result into increased potentially avoidable adverse outcomes that may lead to high morbidity and mortality as well as increased resource utilization in the hospital system of care. Therefore, timely recognizing and reporting of medication errors will help to identify the possible causes and formulate good strategies to avoid the error in future. Although the institution has implemented continuous quality improvement programs that focus on systems, rather than individuals, barriers remain in medication administration error reporting. It is critical that not only the data, but the reporting processes themselves, be carefully evaluated as part of any quality improvement initiative. While it is unrealistic to expect a zero-error rate, a culture that supports identification and reporting of adverse events (one that drives out fear) will enhance quality improvement initiatives. However, the system of care generated about medication errors reporting and identifying the possible causes of error should be basically made for improvement for individual and the system at large trying also to remove the fear when someone reports the error. The hospital must adopt the WHO guideline for medication errors as well protocol, there should also an incident report book for a medication error in every unit.
Ethics Approval and Consent to Participate
Prior to the study ethical approval was obtained from the Ethical Review Board of Jakaya Kikwete Cardiac Institute (JKCI). An official letter from the executive director of JKCI was taken to get the permission to collect data from the hospital then distributing the questionnaires to the study participants. Permission to conduct training was obtained and supervised by research and training department. All methods were carried out in accordance with relevant guidelines and regulations.
However, an informed consent was obtained from all the participants of this study. The participants were explained about the component of the tool and how to fill the required data and they were reassured that the information collected would be kept confidentially and used for study purpose only.
Consent for Publication
Not applicable.
Availability of Data and Materials
All data extracted and analysed in this study have all collected and accumulated in this paper. The information to support the results of this paper are available to the corresponding author just in case they are needed.
Competing Interest
Authors have declared that no competing interests exists.
Funding Sources
There was no source of fund in this particular study.
Author Contributions
A.N. study design, wrote and prepared the original draft of the manuscript and is the corresponding author. Reviewed and edited the manuscript. S.K. assisted in study design, statistical analysis and interpretation of data. N.M. assisted in data collection and analysis. R.M. arrangement of the manuscript. All authors read and approved the final manuscript.
Acknowledgement
We thank the nurses of Jakaya Kikwete Cardiac Institute working inpatients and intensive care units for their acceptance of participating in this study. We also appreciate the contribution and support from research and training department of Jakaya Kikwete Cardiac Institute.
References
1. M. Garrouste-Orgeas Outcomerea Research Group, 75019 Paris, France; Understanding medical errors and adverse events in ICU patients. 2016; 42:107-109.
2. Arabi, Y. M., Schultz, M. J., & Salluh, J. I. (2017). Intensive Care Medicine in 2050: global perspectives. Intensive Care Medicine, 43, 1695-1699.
3. Donaldson, M. S., Corrigan, J. M., & Kohn, L. T. (Eds.). (2000). To err is human: building a safer health system.
4. Counsel of Europe (2010) Partial agreement in the social and public health field .Survey on medication errors. Strasbourg. Strasbourg 341, 392.
5. ICU physician staffing (2010) Fact sheet. The Leapfrog group for patient safety rewarding higher standards 340, 390.
6. Valentin, A., Capuzzo, M., Guidet, B., Moreno, R., Metnitz, B., & Bauer, P. (2009). Errors in administration of parenteral drugs in intensive care units: multinational prospective study. Bmj, 338.
7. Fahimi, F., SISTANI, Z. M., Abrishami, R., & BANI, A. S. (2007). An observational study of errors related to the preparation and administration of medications given by infusion devices in a teaching hospital.IJPR, 295-299.
8. Williams, D.J.P. (2007) Medication errors. JR Coll Physicians Edinb 37, 343-346.
9. Moyen, E., Camiré, E., & Stelfox, H.T. (2008). Clinical review: medication errors in critical care. Critical care, 12(2), 1-7.
10. Barker, K. N., Flynn, E. A., Pepper, G. A., Bates, D. W., & Mikeal, R. L. (2002). Medication errors observed in 36 health care facilities. Archives of internal medicine, 162(16), 1897-1903.
11. Tissot, E., Cornette, C., Limat, S., Mourand, J. L., Becker, M., Etievent, J. P., & Woronoff-Lemsi, M. C. (2003). Observational study of potential risk factors of medication administration errors. Pharmacy world and science, 25, 264-268.
12. Schneider, M. P., Cotting, J., & Pannatier, A. (1998). Evaluation of nurses’ errors associated in the preparation and administration of medication in a pediatric intensive care unit. Pharmacy World and Science, 20, 178-182.
13. Camiré, E., Moyen, E., & Stelfox, H. T. (2009). Medication errors in critical care: risk factors, prevention and disclosure. Cmaj, 180(9), 936-943.
14. Mohamed, N., & Gabr, H. (2010). Quality improvement techniques to control medication errors in surgical intensive care units at emergency hospital, Al-Mansoura University, Egypt. Journal of Medicine and Biomedical Sciences, 5, 2073-78.
15. Wilmer, A., Louie, K., Dodek, P., Wong, H., & Ayas, N. (2010). Incidence of medication errors and adverse drug events in the ICU: a systematic review. Quality and Safety in Health Care, 19(5), e7-e7.
16. Goldstein, R.S. (2005). Management of the critically ill patient in the emergency department: focus on safety issues. Critical care clinics, 21(1), 81-89.
17. McBride-Henry, K., & Foureur, M. (2006). Medication administration errors: understanding the issues. Australian Journal of Advanced Nursing, The, 23(3), 33-41.
18.Pepper, G.A. (2008) Errors in drug administration by nurses. Am J Health Syst Pharm, 52(4), 390-395.
19. Leape, L. L., Bates, D. W., Cullen, D. J., Cooper, J., Demonaco, H. J., Gallivan, T., ... & Edmondson, A. (1995). Systems analysis of adverse drug events. Jama, 274(1), 35- 43.
20. Phillips, J., Beam, S., Brinker, A., Holquist, C., Honig, P., Lee, L. Y., & Pamer, C. (2001). Retrospective analysis of mortalities associated with medication errors. American journal of health-system pharmacy, 58(19), 1835-1841.
21. Sabry, N. A., Farid, S., & Aziz, E. (2009). Role of the pharmacist in identification of medication related problems in the ICU: a preliminary screening study in an Egyptian teaching hospital. Aust J Basic Appl Sci, 3, 995-1003.
22. Eslamian, J., Taheri, F., Bahrami, M., & Mojdeh, S. (2010). Assessing the nursing error rate and related factors from the view of nursing staff. Iranian journal of nursing and midwifery research, 15(Suppl1), 272.
23. Agalu, A., Ayele, Y., Bedada, W., & Woldie, M. (2011). Medication prescribing errors in the intensive care unit of Jimma University Specialized Hospital, Southwest Ethiopia. Journal of multidisciplinary healthcare, 377-382.
24. Jimma University Specialized Hospital. Accessed on 15/11/2010 at http://www.ju.edu.et/node/346
25. Franklin, B. D., O’Grady, K., Donyai, P., Jacklin, A., & Barber, N. (2007). The impact of a closed-loop electronic prescribing and administration system on prescribing errors, administration errors and staff time: a before-andafter study. BMJ Quality & Safety, 16(4), 279-284.
26. Pham, J.C., Story, J.L., Hicks, R.W., Shore, A.D., Morlock, L.L., Cheung, D.S., ... & Pronovost, P.J. (2011). National study on the frequency, types, causes, and consequences of voluntarily reported emergency department medication errors. The Journal of emergency medicine, 40(5), 485-492.
27. Simpson, J.H., Lynch, R., Grant, J., & Alroomi, L. (2004). Reducing medication errors in the neonatal intensive care unit. Archives of Disease in Childhood-Fetal and Neonatal Edition, 89(6), F480-F482.
28. Tang, F.I., Sheu, S.J., Yu, S., Wei, I.L., & Chen, C.H. (2007). Nurses relate the contributing factors involved in medication errors. Journal of clinical nursing, 16(3), 447- 457.
29. Kaushal, R., Bates, D.W., Landrigan, C., McKenna, K.J., Clapp, M.D., et al. (2001). Medication errors and adverse drug events in pediatric inpatients. Jama, 285(16), 2114- 2120.
30. Truter, A., Schellack, N., & Meyer, J. C. (2017). Identifying medication errors in the neonatal intensive care unit and paediatric wards using a medication error checklist at a tertiary academic hospital in Gauteng, South Africa. South African Journal of Child Health, 11(1), 5-10.
31. Agalu, A., Ayele, Y., Bedada, W., & Woldie, M. (2012). Medication administration errors in an intensive care unit in Ethiopia. International archives of medicine, 5(1), 15.
32. Valentin, A., Capuzzo, M., Guidet, B., Moreno, R.P., Dolanski, L., et al. (2006). Patient safety in intensive care: results from the multinational Sentinel Events Evaluation (SEE) study. Intensive care medicine, 32(10), 1591–1598.
33. Valentin, A., Capuzzo, M., Guidet, B., Moreno, R., Metnitz, B., et al. (2009). Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ (Clinical research ed.), 338, b814.
34. Vazin, A., Zamani, Z., & Hatam, N. (2014). Frequency of medication errors in an emergency department of a large teaching hospital in southern Iran. Drug, healthcare and patient safety, 6, 179–184.
35. James, J.T. (2013). A new, evidence-based estimate of patient harms associated with hospital care. Journal of patient safety, 9(3), 122–128.
36. Merino, P., Álvarez, J., Cruz Martín, M., Alonso, Á., Gutiérrez, I., et al. (2012). Adverse events in Spanish intensive care units: the SYREC study. International journal for quality in health care : journal of the International Society for Quality in Health Care, 24(2), 105–113.
37. Vazin, A., & Delfani, S. (2012). Medication errors in an internal intensive care unit of a large teaching hospital: a direct observation study. Acta medica Iranica, 50(6), 425- 432.
38. Truter, A., Schellack, N., & Meyer, J.C. (2012) Identifying medication errors in the neonatal intensive care unit and paediatric wards using a medication error checklist at a tertiary academic hospital in Gauteng, South Africa. 2012, 5-10.
39. Lerner, R.B., de Carvalho, M., Vieira, A.A., Lopes, J.M.,& Moreira, M.A.(2008). Medication errors in a neonatal intensive care unit. Jornal de Pediatria 84(4),166-170.
40. Vazin, A. (2016). Medication errors in Pediatric Intensive Care Unit: incidence, types and outcome. Trends Pharmaceutical Sciences 2(2), 109-116.
41. Allen, I.E, & Seaman, C.A. (2007). Likert scale and data analysis. Quality Progress, 40(7), 64-65.
42. Awang, Z. Afthanorhan, A., & Mamat, M. (2016). The likert scale analysis using parametric based structural Equation modeling. Computational Method Social Sci 4(1),13.
43. Boone, H.N., & Boone, D.A. (2012). Analyzing Likert scale. J Extension, 50(2), 1-5.
44. Josh, A., Kale, S., Chandel, S., & Pal, D.K. (2015). Likert scale explored and explained. British J Appl Science Technol 7(4), 396.
45. Shahrokhi, A., Ebrahimpour, F., & Ghodousi, A. (2013). Factors effective on medication errors: A nursing view. Journal of research in pharmacy practice, 2(1), 18–23.
46. Shitu, Z., Aung, M. M.T., Tuan Kamauzaman, T. H., & Ab Rahman, A. F. (2020). Prevalence and characteristics of medication errors at an emergency department of a teaching hospital in Malaysia. BMC health services research, 20(1), 56.
47. Stratton, K. M., Blegen, M. A., Pepper, G., & Vaughn, T. (2004). Reporting of medication errors by pediatric nurses. Journal of pediatric nursing, 19(6), 385–392.
48. Poorolajal, J., Rezaie, S., & Aghighi, N. (2015) Barriers to medical error reporting. Int J Prev Med 6, 97.
49. Masoumeh, S., & Hamed, T. Factors Affecting Medication Errors from the Perspective of Nursing Staff.
50. Cramer, H., Pohlabeln, H., & Habermann, M. (2013) Factors causing or influencing nursing errors as perceived by nurses: findings of a cross-sectional study in German nursing homes and hospitals. J Public Health, 21(2), 145- 153.
51. Feleke, S. A., Mulatu, M. A., & Yesmaw, Y. S. (2015). Medication administration error: magnitude and associated factors among nurses in Ethiopia. BMC nursing, 14, 53.



