Research Article - (2024) Volume 1, Issue 2
Factors that Led to the State Being Unsuccessful in Addressing the Risk of Covid-19
Received Date: Nov 03, 2024 / Accepted Date: Sep 27, 2024 / Published Date: Nov 25, 2024
Abstract
The COVID-19 pandemic, originating in Wuhan, China, in late 2019, swiftly escalated into a global health crisis by March 2020, severely impacting nations worldwide. The World Health Organization (WHO) faced criticism for delayed responses and underreporting, particularly from China, compounded by geopolitical tensions and funding shortages. This constrained the WHO's ability to effectively manage the pandemic. Additionally, national responses varied significantly, influencing outcomes. Key factors contributing to the state's failure to address COVID-19 effectively include delayed government actions, governance and leadership failures, poor communication, and inadequate economic support. Early and stringent measures, as demonstrated by New Zealand, resulted in better outcomes compared to countries like Italy and the United States, which experienced severe outbreaks due to delayed responses and inconsistent communication. Governance issues, such as the lack of cohesive strategies and leadership coordination, were evident in countries like Indonesia and Japan, leading to inconsistent policy implementation and poor outcomes. Economic support measures played a critical role in public compliance and economic stability. Countries like the UK provided substantial financial aid, yet disparities in support led to ongoing struggles for low-income families. In contrast, countries in the Global South faced significant challenges in providing adequate economic support, exacerbating existing inequalities and complicating pandemic management. Recommendations for future responses include improving targeted health interventions, enhancing community engagement in policy-making, increasing international financial and technical support, and revising global health treaties to ensure equitable resource access. These steps are essential to build more resilient health systems capable of effectively managing future global health crises.
Introduction
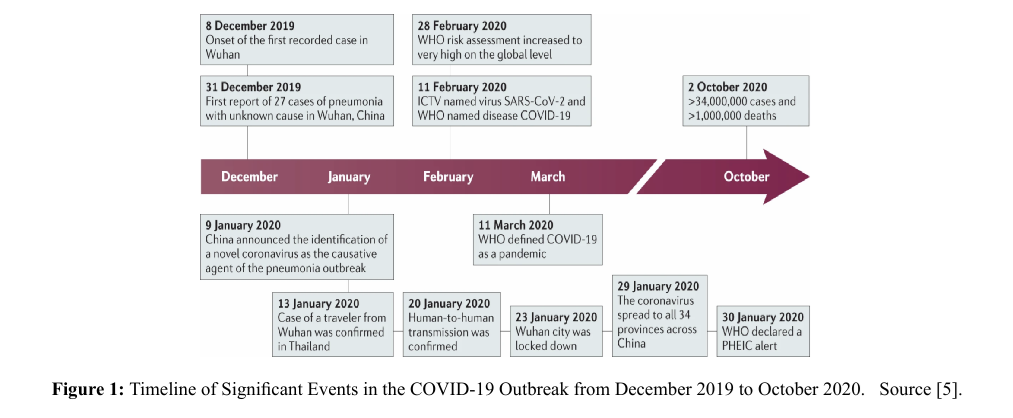
The COVID-19 pandemic emerged as one of the most significant global health crises in recent history, leaving an indelible impact on countries worldwide. [1]. It originated from Wuhan, China, in late 2019, and rapidly spread across the globe, infecting approximately 450 million people and causing 6 million deaths by 2024 [2]. Initially, the disease was referred to as 'Wuhan pneumonia,' before the World Health Organization (WHO) officially declared a pandemic on March 11, 2020 (as shown in Figure 1). By that time, COVID-19 had spread to 114 countries, resulting in over 118,000 confirmed cases and 4,291 deaths globally. Following the declaration, several measures were taken by the WHO to enhance coordination and communication with health authorities worldwide. It also urged all countries to take aggressive actions to combat the virus's spread. However, the virus continued to mutate until late 2022 when it came under control. It is uncertain whether the regression of the pandemic was spontaneous, the result of a coordinated global response, or a combination of both.
There are opinions that the effectiveness in containing the COVID-19 pandemic could have been significantly improved if the WHO had declared it a public health emergency of international concern (PHEIC) much earlier [3]. Critics argue that China misled the WHO by underreporting the extent of community transmission and providing inaccurate figures at the pandemic's onset [4]. Another factor attributed to the delay was geopolitical tensions which undermined its capability to respond swiftly [3]. The WHO faced not only political interference but also funding shortages during the pandemic, which constrained its response capabilities and increased its vulnerability to external influence. For instance, the WHO's COVID-19 Strategic Preparedness and Response Plan (SPRP) for 2020-2021 operated with a budget of $1.96 billion, less than a quarter of the over $7.5 billion the US Centers for Disease Control and Prevention (CDC) received in emergency funding through multiple legislative packages over the same period (WHO, n.d.; CDC, n.d.). These, together with the historical precedents, such as the delayed declaration of a PHEIC during the Ebola outbreak in Africa in 2014, further highlight the need for timely action. Hence, increased political support, legal authority, and financial sustainability are needed to enhance the WHO's effectiveness in managing global health crises.
Even after the WHO declared COVID-19 a pandemic, countries differed in implementing airborne mitigation measures promptly, depending on the capability of their health system to respond to the threat, making some states more successful than others [1]. Although, most governments were thrust into a state of emergency, and have taken decisive action to mitigate the public health threat. The varied responses to the pandemic have highlighted significant differences in the capacity of states to manage such a crisis effectively [1,4]. Above all, the extent and duration of the COVID-19 epidemic have demonstrated the inability of the states to prevent or control its spread. Therefore, this essay aims to critically analyze the myriad factors that have contributed to the states’ failure and why some are better than others in addressing the risks posed by COVID-19.
Country-Level Factors that Contributed to the Inability to Address the Risk Of Covid-19
Delay in Government Response
The effectiveness of a state's response to the COVID-19 pandemic is significantly influenced by the timing of the instituted response measures (Salmon et al., 2021). In other words, the earlier a country responds, its pandemic management is more effective. This finding is supported by Zhang & Enns (2022), whose study modeled China’s response rate to the pandemic by health outcomes. The study revealed that an early response by one week earlier could have averted 35% of the mortality observed during the first wave of the pandemic. This suggests that optimizing the timing of mitigation strategies could significantly reduce the pandemic’s impact. Despite the virus crossing borders, some states were slow to implement critical measures such as lockdowns, mask mandates, and social distancing guidelines. Countries that delayed their responses experienced more severe outbreaks. Italy, the first European country significantly affected, illustrates the consequences of delayed action. Despite warning signs from the outbreak in Wuhan, Italian authorities imposed a partial lockdown in the province of Lodi in Lombardy only on February 21, 2020, following the confirmation of the first COVID-19 cases in Rome on January 31, 2020. By that time, the virus had reached about ten municipalities and affected approximately 50,000 people [6]. It was not until March 9, 2020, that Italy implemented nationwide restrictions, by which time the virus had already spread widely. The lockdown, which ended on May 4, 2020, saw cumulative incidence (CI) rates in Italian regions ranging from less than 5 cases per 100,000 to over 11 cases per 100,000 inhabitants [6]. This delay resulted in a rapid surge of cases, overwhelming the healthcare system and leading to one of the highest mortality rates in the country.
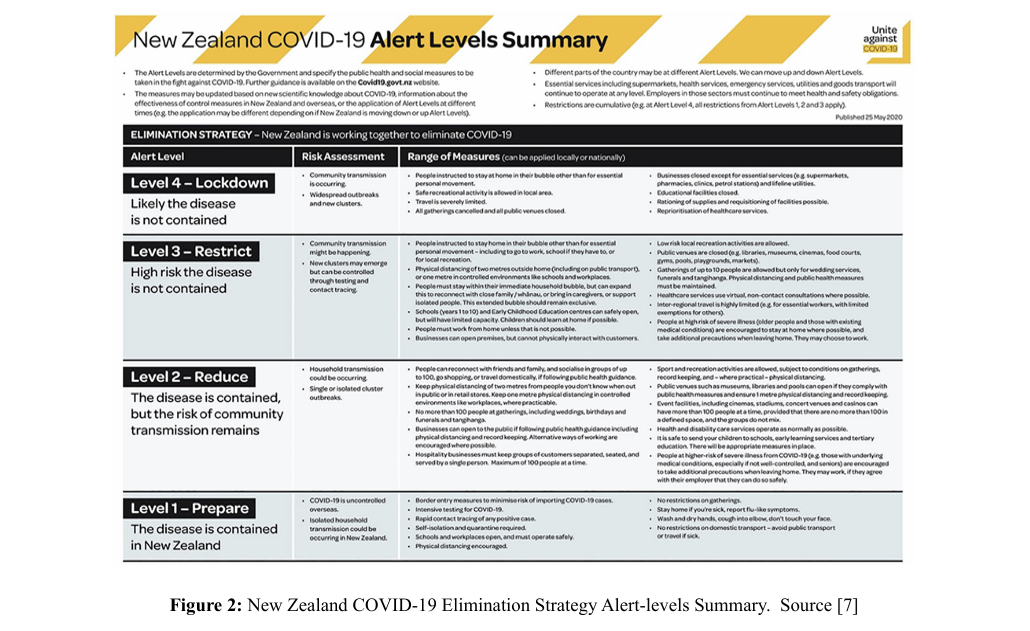
In contrast, New Zealand provides a case study of how structured leadership and prompt response can effectively manage a pandemic. Under Prime Minister Jacinda Ardern's leadership, the state implemented stringent measures early in the pandemic. On March 25, 2020, New Zealand moved to the highest alert level, imposing a nationwide lockdown as part of the “Elimination Strategy Campaign” when it had only 205 confirmed cases and no deaths. New Zealand was the first country to choose “elimination” as a specific policy response [7]. This strategy involved conducting community risk assessments and implementing targeted interventions based on a four-level alert system as shown in Figure 2. This enabled New Zealand to repeatedly eliminate community virus transmission during the pandemic. Through the first 18 months of the pandemic, until vaccines became widely available, New Zealand maintained very low COVID-19 mortality rates, and by June 2020, there were no active cases of the virus [7]. These early interventions were pivotal in controlling the outbreak while minimizing economic disruption and have helped New Zealand achieve relative success compared to many other countries in the world [8]. However, Thornton noted evidence of noncompliance, especially at the initial stages when there was limited knowledge about the pandemic, and institutions had to adapt to various operational changes [9]. As the New Zealand COVID-19 Elimination Strategy was fully implemented, involving widespread testing and the use of technology for efficient contact tracing, there was a marked increase in large-scale compliance.
Governance and Leadership Failures
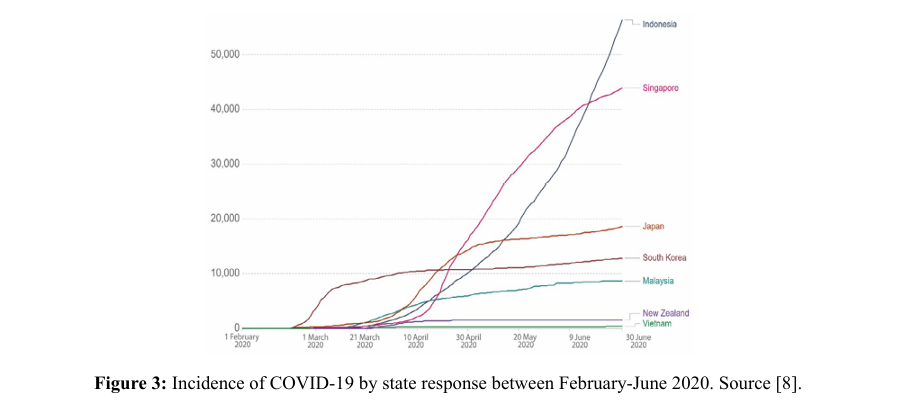
Effective pandemic response requires seamless coordination and leadership between the government, and both central and regional health institutions. However, in many countries, the lack of cohesive strategy and governance between these levels of government severely hampered efforts to combat the virus. This is evident in the Ling study which compared states’ success in addressing the risk of COVID-19 based on the effectiveness of the coordinated response among countries’ health systems that responded within the same time [8]. The study revealed how Vietnam and New Zealand's health system leadership, coupled with effectiveness of coordination of the response have led to better outcomes. Both countries designed principles contributing to high level government stringency and health indices and successfully controlled the virus, as shown in Figure 3. As against Indonesia and Japan associated with the low presence of design principles, were deemed the least successful due to the lack of coordinated central leadership. According to the study, different regions in both countries implemented varying policies, leading to inconsistencies in response measures, while the central government of both countries were hesitating to implement strict measures promptly.
England has also reformed its health systems in response to COVID-19 by the disbandment of Public Health England (PHE) and its replacement with the UK Health Security Agency (UKHSA) to create more specialized and efficient operations [10]. This is in response to the shortcomings in the agency's (health protection) ability to manage such an unprecedented crisis particularly concerning the lack of capacity to test, monitor, and trace the virus effectively [11]. The remaining health improvement and research functions of PHE were distributed into distinct bodies; the Office for Health Improvement and Disparities (OHID) and the National Institute for Health Research (NIHR) [10]. UKHSA is an executive agency (like PHE), that was specifically designed to bring together expertise in health protection, emergency preparedness, and response. However, this restructuring has faced significant criticisms; Hunter argued that the transition, which occurred suddenly and unexpectedly during the ongoing pandemic, disrupted operations and diverted attention from immediate response efforts [12]. Additionally, creating multiple bodies has introduced new layers of bureaucracy, complicating coordination and communication. Critics also point out that structural changes alone are insufficient to address underlying issues in public health capacity without substantial increases in funding and staffing [13]. Evaluations of the UK's pandemic response, particularly in areas such as vaccine rollout, and test and trace programs, suggest that the reorganization has not led to significant improvements. This is evident by the persistent gaps in COVID-19 vaccine coverage across the existing factors associated with health inequalities. According to the National Audit Office, 2022 Report on the rollout of the COVID-19 vaccination program in England, vaccination rates were lower among socio-economically disadvantaged groups (75% for the most deprived decile compared to 94% for the least deprived) and certain minority ethnic groups (48% for individuals of Chinese origin, 49% for those of Black Caribbean and Black Other origin, versus 86% for the white British group) who had 2 doses of the vaccine by July 2021. These challenges highlight the need for continuous evaluation and adaptation of health system reforms to ensure they effectively address public health emergencies.
Lack of Transparency in Communication and Politicization of the Pandemic
Effective communication is fundamental to a robust health system [14]. Clear, consistent, and honest communication builds public trust and ensures compliance with public health measures, which is crucial for managing a pandemic. However, during the COVID-19 pandemic, many governments and health agencies failed to communicate transparently about the risks and uncertainties associated with the virus. This lack of transparency eroded public trust and increased resistance to health directives, significantly hindering efforts to control the spread of the virus.
The United States exemplifies how poor communication exacerbated the public health crisis during the pandemic. The response was marred by conflicting messages from federal and state authorities and inconsistent guidance from health agencies [15]. Discrepancies between data reported by the World Health Organization (WHO) and individual states further fueled confusion. President Trump's downplaying of the virus to present a more favorable situation created additional confusion and undermined public health efforts [3]. Mixed messages from different levels of government, often contradicting health experts, led to widespread non-compliance with health measures, contributing to one of the highest morbidity and mortality rates globally. Haeder & Gollust highlighted that the lack of a unified national strategy and the politicization of health measures, such as mask-wearing and social distancing, eroded public trust and compliance, leading to widespread outbreaks and a high death toll [16].
During the first wave of the pandemic, nearly a quarter of global deaths occurred in the United States [17]. Ker examined the polarization among the US public in two national studies, revealing that participants placed less trust in politicians to handle the pandemic and more trust in medical experts, such as the WHO, and found that rapid spread of misinformation and rumors, especially through social media, compounded the challenge of effective communication. False claims about the origins of the virus, the efficacy of treatments, and vaccine safety created significant barriers to public compliance with health measures. Furthermore, debates about the pandemic being part of a global vaccine conspiracy and claims that it was created by Bill Gates led to significant public distrust [18]. Increased partisan media facilitated the spread of mistrust among the population, exacerbating the problem [18]. As a result, effective pandemic response efforts were hindered, highlighting the crucial need for accurate and unified public health information. In contrast, countries that acted swiftly and communicated clearly with their populations were generally more successful in controlling the virus. New Zealand exemplifies best practices in this area. The government provided regular, detailed updates on the situation and the measures being taken, ensuring transparency and maintaining public trust [19]. The Ministry of Health, with a high degree of autonomy, along with the COVID-19 Response Minister and the Director-General of Health, were prominent figures in managing and communicating the country's response to the pandemic thereby enabling a coordinated and proactive approach [8].
Lack of Economic Support/Incentives
The implementation of economic support measures has been essential in mitigating the economic impact of the pandemic and ensuring compliance with public health measures [20]. In other words, the extent to which states have been able to provide economic support and address social inequalities has influenced both public compliance and overall resilience to the pandemic. During the lockdowns, various countries provided financial support to alleviate financial distress, ranging from stimulus payments, unemployment benefits, business grants, and support for healthcare systems. Generally, countries that provided robust economic support to individuals and businesses affected by lockdowns and restrictions saw better compliance with public health measures and reduced economic hardship. For example, the UK implemented several economic stimulus packages, including direct payments to individuals and enhanced unemployment benefits. It spent £180 billion supporting businesses and £129 billion on loans and guarantees since the first lockdown in March 2020, with slight revisions during subsequent COVID-19 waves [21]. The bulk of the support came through the Coronavirus Job Retention Scheme (CJRS/furlough) and the Self-Employment Income Support Scheme (SEISS), while many business support schemes were administered by local authorities, who had some f lexibility in determining how to allocate resources [22]. These measures helped stabilize the economy and support households and businesses during periods of reduced economic activity.
However, despite these measures, many low-income families struggled as the assistance did not always match their living costs and needs [21]. Additionally, the urgency to disburse funds quickly led to insufficiently rigorous verification processes, making it easier for fraudulent claims to slip through. Some individuals and businesses made false claims to access financial support schemes, including exaggerating losses, claiming support for non-existent employees, and misrepresenting business activities to qualify for aid. There is evidence that the pandemic has exacerbated existing inequalities, and financial aid did not sufficiently address this gap in the UK [23]. The pandemic has exposed pre-existing social inequalities, leading to differential impacts on vulnerable populations. Factors such as income, race, ethnicity, occupation, housing, and access to healthcare have all influenced the risk of exposure to the virus and the severity of its outcomes [23]. As a result, UK support programs were beneficial, however, implementing more robust systems for verifying claims and detecting fraud would have reduced the misuse and abuse of the programs.
Additionally, countries in the Global South, such as India and Brazil, struggled to provide insufficient economic support to vulnerable populations, leading to widespread hardship, protests, and compliance with preventive measures [24]. There was evidence suggesting that the lack of comprehensive social safety nets exacerbated existing inequalities and hindered the ability of governments to control the spread of the virus. Additionally, the disparities in the distribution and adequacy of financial support have influenced public compliance with health measures and have impacted the overall resilience of the population to the pandemic [25].
Recommendations
Several recommendations can be made to enhance future pandemic responses within and between the states:
1. Recommendation for states to improve in-country future pandemic response:
• Countries should implement more targeted health interventions aimed at vulnerable populations to address disparities in healthcare access and outcomes. This includes providing additional support to low-income communities, ethnic minorities, and those in precarious employment.
• LMICs should consider improving the active engagement of community leaders and representatives in the policy-making process, especially concerning large-scale epidemiological interventions to ensure that interventions are culturally sensitive and equitable. This will help in developing more inclusive health policies that consider the diverse needs of different population groups.
2. Recommendations for global health organizations to improve inter-country response:
• International aid and partnerships with global health organizations like WHO should increase financial and technical support to low-income countries to strengthen their health systems and pandemic preparedness, reducing risks like the vaccine delays seen in Sub-Saharan Africa during COVID-19.
• The INB and World Health Assembly should revise the pandemic treaty to balance national sovereignty with international obligations, ensuring equitable resource access and addressing the differing needs of low- and high-income countries. The pandemic transcends politics, and true safety is only achieved when everyone is protected.
Conclusion
The COVID-19 pandemic exposed global health system weak nesses and areas needing improvement. Failures in communica tion, geopolitical tensions, and lack of coordination, contributed to states' inability to manage the pandemic effectively. To enhance future pandemic responses, states should adopt a comprehensive approach, depoliticizing health responses, improving communica tion, addressing socioeconomic disparities, and ensuring equita ble resource distribution. These measures will build more resilient health systems for managing future crises [26-42].
Funding
Conflict of Interest: No conflict of interest.
Data Availability Statement
Data sharing is not applicable as no new data were created.
References
1. Shamasunder, S., Holmes, S. M., Goronga, T., Carrasco, H., Katz, E., Frankfurter, R., & Keshavjee, S. (2020). COVID-19 reveals weak health systems by design: why we must re make global health in this historic moment. Global Public Health, 15(7), 1083-1089.
2. Phua, K. L. (2014). Measuring Health System Performance: A critique, with proposals for improving on the WHO “Building Blocks Framework”. The Open Public Health Journal, 7(1).
3. Schismenos, S., Smith, A. A., Stevens, G. J., & Emmanouloudis, D. (2021). Failure to lead on COVID-19: what went wrong with the United States?. International Journal of Public Leadership, 17(1), 39-53.
4. Brown, R. B. (2020). Public health lessons learned from biases in coronavirus mortality overestimation. Disaster medicine and public health preparedness, 14(3), 364-371.
5. Hu, B., Guo, H., Zhou, P., & Shi, Z. L. (2021). Characteristics of SARS-CoV-2 and COVID-19. Nature reviews microbiology, 19(3), 141-154.
6. Bosa, I., Castelli, A., Castelli, M., Ciani, O., Compagni, A., Galizzi, M. M., ... & Vainieri, M. (2022). Response to COVID-19: was Italy (un) prepared?. Health Economics, Policy and Law, 17(1), 1-13.
7. Jamieson, T. (2020). “Go hard, go early”: Preliminary lessons from New Zealand’s response to COVID-19. The American Review of Public Administration, 50(6-7), 598-605.
8. Ling, G. H. T., Md Suhud, N. A. B., Leng, P. C., Yeo, L. B., Cheng, C. T., Ahmad, M. H. H., & Ak Matusin, A. M. R. (2021). Factors influencing Asia-Pacific countries’ success level in curbing COVID-19: A review using a social ecological system (SES) framework. International journal of environmental research and public health, 18(4), 1704.
9. Thornton, K. (2021). Leading through COVID-19: New Zealand secondary principals describe their reality. Educational Management Administration & Leadership, 49(3), 393-409.
10. O’Dowd, A. (2021). New agency will focus on preparing and protecting UK from future pandemics..
11. Calvert, J., & Arbuthnott, G. (2021). Failures of state: The inside story of Britain’s battle with coronavirus. HarperCollins.
12. Hunter, D. J., Littlejohns, P., & Weale, A. (2022). Reforming the public health system in England. The Lancet Public Health, 7(9), e797-e800.
13. Littlejohns, P., Hunter, D. J., Weale, A., Johnson, J., & Khatun, T. (2023). Principles and process in the new public health settlement. In Making Health Public (pp. 58-76). Policy Press.
14. Borghi, J., & Brown, G. W. (2022). Taking systems thinking to the global level: using the WHO building blocks to describe and appraise the global health system in relation to COVIDâ?19. Global Policy, 13(2), 193-207.
15. Galaitsi, S. E., Cegan, J. C., Volk, K., Joyner, M., Trump, B. D., & Linkov, I. (2021). The challenges of data usage for the United States’ COVID-19 response. International Journal of Information Management, 59, 102352.
16. Haeder, S. F., & Gollust, S. E. (2020). From poor to worse: Health policy and politics scholars’ assessment of the US COVIDâ?19 response and its implications. World Medical & Health Policy, 12(4), 454-481.
17. Amu, H., Dowou, R. K., Saah, F. I., Efunwole, J. A., Bain, L. E., & Tarkang, E. E. (2022). COVID-19 and health systems functioning in sub-Saharan Africa using the “WHO Building Blocks”: the challenges and responses. Frontiers in Public Health, 10, 856397.
18. Motta, M., Stecula, D., & Farhart, C. (2020). How right leaning media coverage of COVID-19 facilitated the spread of misinformation in the early stages of the pandemic in the US. Canadian Journal of Political Science/Revue canadienne de science politique, 53(2), 335-342.
19. Wilson, S. (2020). Pandemic leadership: Lessons from New Zealand’s approach to COVID-19. Leadership, 16(3), 279 293.
20. Nicola, M., Alsafi, Z., Sohrabi, C., Kerwan, A., Al-Jabir, A., Iosifidis, C., ... & Agha, R. (2020). The socio-economic implications of the coronavirus pandemic (COVID-19): A review. International journal of surgery, 78, 185-193.
21. Greene, F. (2022). Scottish Covid-19 Inquiry: Research Commission: Financial and Welfare Support to Businesses and Individuals.
22. Institute for Government. (2020) Coronavirus: Economic support for individuals.
23. Blundell, R., Cribb, J., McNally, S., Warwick, R., & Xu, X. (2021). Inequalities in education, skills, and incomes in the UK: The implications of the COVID-19 pandemic. Institute for Fiscal Studies, 1-42.
24. Chowdhury, A. Z., & Jomo, K. S. (2020). Responding to the COVID-19 pandemic in developing countries: lessons from selected countries of the global south. Development, 63(2), 162-171.
25. Tan, S. Y., De Foo, C., Verma, M., Hanvoravongchai, P., Cheh, P. L. J., Pholpark, A., ... & Legido-Quigley, H. (2023). Mitigating the impacts of the COVID-19 pandemic on vulnerable populations: Lessons for improving health and social equity. Social Science & Medicine, 328, 116007.
26. Adedeji-Adenola, H., Olugbake, O. A., & Adeosun, S. A. (2022). Factors influencing COVID-19 vaccine uptake among adults in Nigeria. PloS one, 17(2), e0264371.
27. Adebisi, Y. A., Rabe, A., & Lucero-Prisno III, D. E. (2021). Risk communication and community engagement strategies for COVID-19 in 13 African countries. Health Promotion Perspectives, 11(2), 137.
28. Afolabi, A. A., & Ilesanmi, O. S. (2021). Addressing COVID-19 vaccine hesitancy: Lessons from the role of community participation in previous vaccination programs. Health promotion perspectives, 11(4), 434.
29. Alenoghena, I. O., & Omuemu, V. O. (2022). The Role of the Ward Health System in COVID-19 Pandemic Response in Nigeria: A Case Study of Edo State. Journal of Community Medicine and Primary Health Care, 34(3), 12-23.
30. Ball, I. (2021). Burning the buffer: New Zealand's budgetary response to COVID-19. Journal of Public Budgeting, Accounting & Financial Management, 33(1), 95-105.
31. Bello, U., Ja’afar, I. K., Ogbolosingha, A. J., Isa, A., Muhammad, J. H., & Abubakar, A. H. (2024). Knowledge, attitude, and practice of COVID-19 screening and vaccine uptake among women attending Maimusari Primary Healthcare in Jere Local Government, North East, Nigeria. Alexandria Journal of Medicine, 60(1), 26-37.
32. Centers for Disease Control and Prevention (n.d.) FY 2021 Congressional Justification. Available at: https://www. cdc.gov/budget/fy2021/congressional-justification.html. Accessed on: 02/06/2024.
33. Crampton, P., Matheson, D., & Cotter, M. (2020). Assessing the design and capability of our publ ic health system in a Covid and post-Covid New Zealand. Policy Quarterly, 16(3).
34. Darne, V.G., Kanthale, A.S. and Shah, F.A., 2023. REVIEW ON CORONAVIRUS DISEASE AND CHARACTERISTICS OF SARS–COV–2. Nat Rev Microbiol. p19(3):141-154.
35. Lenharo, M. (2024). Hope for global pandemic treaty rises— despite missed deadline. Nature, 630(8016), 282-282.
36. Levin, A. T., Owusu-Boaitey, N., Pugh, S., Fosdick, B. K., Zwi, A. B., Malani, A., ... & Meyerowitz-Katz, G. (2022). Assessing the burden of COVID-19 in developing countries: systematic review, meta-analysis and public policy implications. BMJ Global Health, 7(5), e008477.
37. Mawani, F. N., Gunn, V., O’Campo, P., Anagnostou, M., Muntaner, C., Wanigaratne, S., ... & An, A. (2021). COVID-19 economic response and recovery: a rapid scoping review. International Journal of Health Services, 51(2), 247 260.
38. National Audit Office UK, The rollout of the COVID-19 vaccination programme in England (2022).
39. National Primary Healthcare Development Agency (NPHCDA) (2022). Primary Healthcare Guidelines. National Primary Healthcare Development Agency.
40. Rao, K., Verma, P., Kumar, K., Verma, M. K., Siddiqui, A. H., Singh, S., ... & Aryal, S. (2020). Review on Newly Identified Coronavirus and its Genomic Organization.
41. Rod, J. E., Oviedo-Trespalacios, O., & Cortes-Ramirez, J. (2020). A brief-review of the risk factors for covid-19 severity. Revista de saude publica, 54, 60.
42. Lancet, T. (2024). The Pandemic Treaty: shameful and unjust. Lancet (London, England), 403(10429), 781.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.