Research Article - (2025) Volume 3, Issue 4
Factors for Plastic Bottle Cap Opening in People with Cervical Spondylotic Myelopathy
2Graduate School, Yamagata Prefectural University of Health Sciences, Japan
Received Date: Mar 04, 2025 / Accepted Date: Apr 03, 2025 / Published Date: Apr 07, 2025
Copyright: ©2025 Yumi Suzuki, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Suzuki, Y., Fujii, H. (2025). Factors for Plastic Bottle Cap Opening in People with Cervical Spondylotic Myelopathy. Eng OA, 3(4), 01-07.
Abstract
Many patients with cervical spondylotic myelopathy (CSM) who are eligible for occupational therapy complain difficulty in using their hands and numbness or pain in their upper and lower limbs, which significantly affect their activities of daily living. Such an inconvenience rapidly increases when they have difficulty opening plastic bottle caps. Therefore, this study investigated the factors for opening plastic bottle caps by evaluating the plastic bottle cap–opening availability status, hand sensation, maximum grip strength, maximum pulp pinch strength, and results of the 10-s grip–release test, which consists of finger flexion and extension for 10 s at maximum effort in people with indications for surgery. The study included 141 patients who met the selection criteria out of 147 patients diagnosed with CSM and indicated for surgery and who were prescribed occupational therapy. The participants were divided into two groups: one group consisting of patients who could open plastic bottle caps 3 weeks after surgery (n = 94) and the other group consisting of those who could not (n = 47). Logistic regression analysis revealed only the average pinch force with an odds ratio of 4.668 (95% confidence interval 2.618–8.322, p = 0.001). In the ROC analysis, the cutoff value for the average pinch force required to open plastic bottle caps was 2.4 kgf. These findings indicated that the MPPS was below 2.4 kgf and that the patient had difficulty opening the plastic bottle caps, which may interfere with their activities of daily living and may be an indication for surgery.
Keywords
Cervical Spondylotic Myelopathy, Pinch Strength, Plastic Bottle Cap Opening
Introduction
To date, cervical spondylotic myelopathy (CSM) has not yet been clearly defined. However, the concept of compression myelopathy is becoming widespread. The guidelines state that “CSM is a general term for diseases in which spinal cord compression caused by age related changes (posterior osteophytes, disc narrowing, and posterior bulging) in a narrow cervical spinal canal, combined with anterior posterior flexion instability and minor trauma of the cervical spine, leads to spinal cord paralysis” CSM commonly results from spinal cord compression between the C5 and C6 vertebrae [1,2]. The functional segment located there is the anterior horn of C7; thus, the dexterous movements of the fingers are impaired. People with CSM have difficulty performing activities of daily living, such as fastening buttons or opening plastic bottle caps. These patients are less likely to respond to conservative treatment once symptoms of spinal paralysis appear; furthermore, delayed surgical timing and paralysis progression lead to poor symptom improvement after surgery [3,4].
CSM is highly prevalent in men aged over 50 years. In Japan, the incidence of CSM requiring treatment is reportedly several cases per 100,000 population [1]. The aging population of this country is rapidly growing; thus, an increase in the number of CSM cases requiring medical treatment is expected [5]. Many patients who are eligible for occupational therapy complain of “difficulty using their hands, which makes their lives inconvenient,” along with numbness or pain in the upper and lower limbs [6]. Such an inconvenience rapidly increases when the patient is unable to open plastic bottle caps [7-12]. During this time, the attending physician often changes the treatment course from conservative to surgical therapy. Consequently, this study investigated the factors for plastic bottle cap opening by evaluating the plastic bottle cap–opening availability status, hand sensation, muscle strength, and repetitive movements in people with indications for surgery.
Participants and Methods
The study included 141 patients (86 men, 55 women; mean age 67.4 ± 11.6 [range, 38–87] years old) who met the selection criteria out of 147 patients diagnosed with CSM and indicated for surgery and who were prescribed occupational therapy at Okitama General Hospital, Yamagata, Japan (Figure 1). Ethics Review Board of Public Okitama General Hospital (approval number: − 28143).Written informed consent was obtained from all participants, written and oral explanations of the purpose and methods of the study and obtained consent.
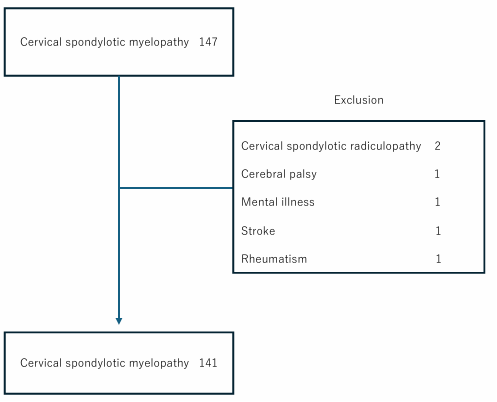
Figure 1: Flow Diagram
The exclusion criteria were the presence of central or peripheral 1 1 1 1 Technologies, Tokyo), and a pinch strength measurement program neurological diseases other than CSM, the inability to understand the examination procedures, and an unstable after surgery general condition.
The occupational therapists interviewed the participants on the day before surgery and on after surgery days 7, 14, and 21 to determine the presence and location of numbness. The participants completed sensory tests, grip and pinch strength measurements, the 10-s grip–release test (10-s test) [13], and a test to open a plastic bottle. In the pinch strength measurement, the participants were instructed to maintain pinching with maximum strength with the thumb and index fingers for 10 s (maximum pulp pinch strength [MPPS]). To measure grip strength, the participants were instructed to hold a Smedley-type grip sensor with their thumb and four fingers and maintain maximum strength for 10 s (maximum grip strength [MGS]). To measure pinch strength, the participants were instructed to pinch the items with their thumb and index f inger as hard as possible for 10 s MPPS. The MGS and MPPS were measured thrice, and the integrated average values over 10 s were used.
The equipment used were a Smedley-type grip strength sensor, a small sensor and indicator EG-210, SPR-6720, EG-220 (Sakai Medical Co., Ltd., Tokyo), a personal computer (Dell (Gigatech, Osaki). The 10-s test consisted of finger flexion and extension for 10 s at maximum effort [13]. The presence, degree, and location of numbness in the fingers were determined. For the test of plastic bottle cap opening, a Green Tea PET bottle (Iyemon, Suntory Holdings Limited, Osaka) was used, and the participants were instructed to open it with their thumb and index fingers. The criterion for the plastic bottle cap opening was 10 s from the start, and switching between the left and right hands was prohibited.
Statistical analysis was conducted using the corresponding Student’s T-test. Logistic regression analysis was conducted using age, MGS, MPPS, sensory test, and 10-s test values as independent variables and whether the plastic bottle cap was opened as a dependent variable. The extracted items were subjected to ROC analysis. The statistical significance level was set to 5%
Results
The MGS on the day before surgery and after surgery days 7, 14, and 21 is presented in Figure 2. On the day before surgery, the MGS, to approximately 10.0 kgf and then gradually decreased after about 5.9 s. Meanwhile, on after surgery day 7, the MGS was maintained after increasing to approximately 15.0 kgf. This characteristic was observed during after surgery days 14 and 21.
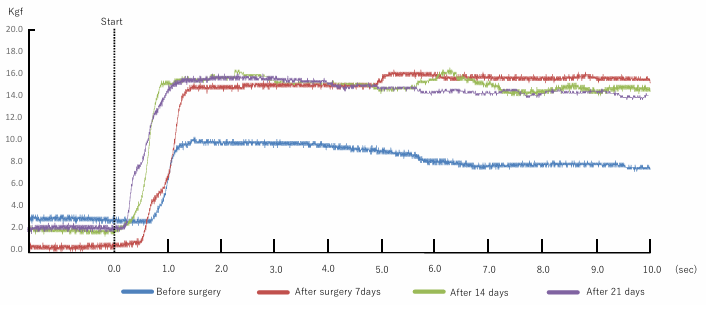
Figure 2: Maximum Grip Strength (MGS) on the Day Before Surgery and on After Surgery Days 7, 14, and 21 (Case A)
Figure 3: Maximum Pulp Pinch Strength (MPPS) on the Day Before Surgery and on After Surgery Days 7, 14, and 21 Case A
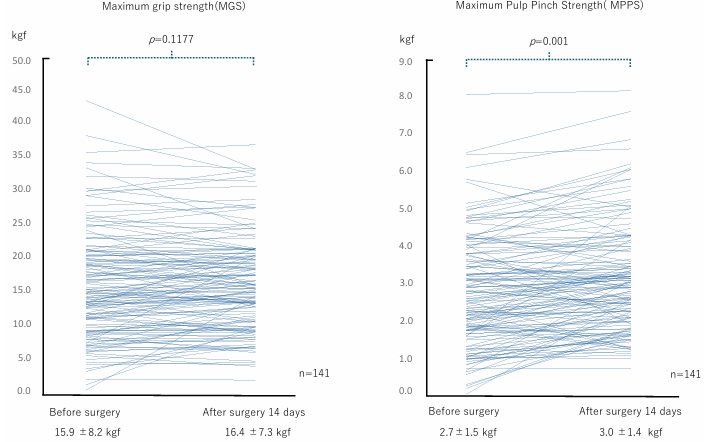
Figure 4: Comparison of the MGS and MPPS Between the Day before Surgery and on After Surgery day 14
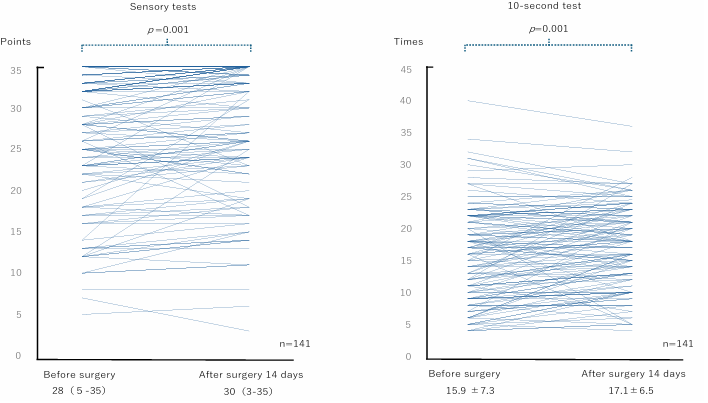
Figure 5: Comparison of Sensory and 10-s Tests on the Day Before Surgery and on After Surgery Day 14
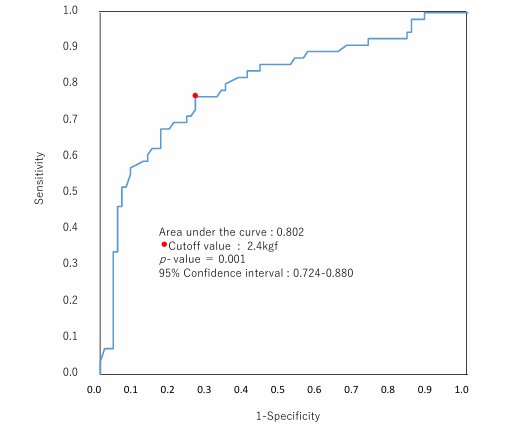
Figure 6: ROC Analysis of the Pinch Strength Required to Open the Plastic Bottle Cap
Furthermore, the MPPS on the day before surgery and on after surgery days 7, 14, and 21 is presented in Figure 3.
The MPPS on the day before surgery showed a delay of approximately 1.8 s from the start cue after the value gradually increased, reaching about 2.0 kgf. Subsequently, the MPPS increased or decreased by approximately 0.5 kgf and gradually decreased after 7.2 s.
On after surgery day 7, the MPPS exhibited a delay of approximately 0.8 s after the cue to begin the task, after which the value gradually increased, reaching approximately 2.0 kgf. Thereafter, the MPPS gradually increased with repeated increases and decreases, reaching approximately 3.0 kgf at 8.2 s. The delay between the cue and the start of the MPPS was smaller on after surgery day 14 than on after surgery day 7. Moreover, the pinch strength values rapidly increased, reaching approximately 3.0 kgf. The MPPS repeatedly increased and decreased, and the pinch strength values remained unchanged until the end of the task.
On after surgery day 21, the MPPS rapidly increased from the start cue and reached approximately 3.2 kgf. Thereafter, the MPPS repeatedly increased and decreased, reaching approximately 3.5 kgf after approximately 3.6 s. Although the pinch strength values remained stable until about 5.8 s after about 6.0 s, the task was completed with repeated increases and decreases of approximately 0.3 to 0.5 kgf.
A comparison of MGS and MPPS between the day before surgery and after surgery day 14 in all participants is presented in Figure 4. The MGS was 15.9 ± 8.2 kgf on the day before surgery and 16.4 ± 7.3 kgf on after surgery day 14, indicating no significant difference between the periods. Meanwhile, the MPPS was 2.7 ± 1.5 kgf on the day before surgery and 3.0 ± 1.4 kgf on after surgery day 14, indicating a significant difference (p = .001).
A comparison of the sensory and 10-s test between the day before surgery and after surgery day 14 in all the participants is presented in Figure 5. The sensory tests showed a significant difference of 28 points (minimum 5 points, maximum 35 points) on the day before surgery and 30 points (minimum 3 points, maximum 35 points) on after surgery day 14th (p = .001) The 10-s test showed a significant difference of 15.9 ± 7.3 times on the day before surgery and 17.1 ± 6.5 times on after surgery day 14 (p = .001).
The study participants were divided into two groups: one consisting of patients who could open the plastic bottle cap 3 weeks after surgery (n = 94) and the other group consisting of patients who could not (n = 47). Logistic regression analysis revealed only the MPPS with an odds ratio of 4.668 (95% confidence interval 2.618–8.322, p = 0.001) (Table 1). In the ROC analysis, the cutoff value for the average MPPS required to open the plastic bottle cap was 2.4 kgf (Figure 6).
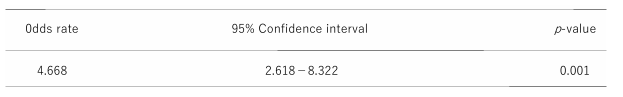
Table 1: Logistic Regression Analysis Revealed the Average Pinch Strength
Discussion
The number of participants in the author’s occupational therapy program for CSM rapidly increased when the patients began having difficulty opening plastic bottle caps. To explore this factor, the authors used sensory tests, MGS, MPPS, the 10-s test, and a test of plastic bottle cap opening on the day before surgery and on after surgery days 7, 14, and 21.
On after surgery day 7, MGS recovery was clear, as in the participant shown in Figure 2, although the surgical effects remained. Meanwhile, the recovery of the MPPS, which is used in daily life, was slow. Strength generation by the Smedley-type grip strength meter mainly occurs by the opposition of the thumb ball and the four fingers [14-16]. Furthermore, the generation of MPPS with small sensors requires holding the thumb in an abduction and internal rotation position at the carpometacarpal joint of the thumb and bringing the thumb and index finger bellies face-to-face [17].
Then, opposing strengths must be generated while holding the small sensor with the thumb and index fingers. These findings indicate that the regulatory strengths for holding the small sensor are superimposed while maintaining the MPPS. Our daily activities are full of object manipulations using the thumb and index fingers, such as opening a sachet and closing a zipper. The thumb and index fingers not only exert pinch strength but are also involved in the object manipulation. In this study, the occupational therapist analyzed the participants’ hand shape and hand movements in detail and provided the necessary guidance [18].
Owing to the residual surgical effects, participant data could not be obtained for this measurement on after surgery day 7. Therefore, we compared before surgery and after surgery day 14, where data could be obtained from the participants on all examination and measurement items. The results indicated improvement in the sensory tests, the 10-s test, and MPPS compared to before surgery. However, no improvement in grip strength was observed. Grip strength is used as a measure of overall muscle strength and an indicator of the progression of various diseases, particularly among the elderly [19-26]. Grip strength measurement is also a standard measure in occupational therapy for CSM. As shown in Figure 2, grip strength improved 1 week after surgery compared with that before surgery. However, Figure 4 shows no significant difference between MGS on the day before surgery and after surgery day14. In addition, no MGS were extracted in the logistic regression analysis. These findings suggest that grip strength is not an indicator for determining a factor in plastic bottle cap opening.
The results of the sensory and 10-s tests as well as the MPPS improved after surgery day 14 compared with that before surgery. However, the latter was extracted from the logistic regression analysis. Therefore, we conducted an ROC analysis between the MPPS and the openability of PET bottle caps and found that the cutoff value for the MPPS was 2.4 kgf. The MPPS cut-off value is an indicator to sharing the need to surgery with patients and their physicians during before surgery evaluation of CSM patients. If the MPPS is less than 2.4 kgf on after surgery day 14, the occupational therapist should work with the patient to facilitate the use of self-help devices for activities of daily living. In other words, the MPPS cutoff be able to be used to evaluate function in patients undergoing conservative treatment for surgery. These f indings suggest that the MPPS is below 2.4 kgf and that the patient may have difficulty opening the plastic bottle caps, which may interfere with their activities of daily living and may be an indication for surgery.
Limitations and Prospects of the Study
This study was conducted on patients at a single institution. Moreover, the patients were treated with multiple surgical techniques. However, we have not investigated the impact of recovery by procedure. In the future, we will investigate and report on the above.
Acknowledgements
The authors sincerely thank Dr. Masahiro Hayashi for his cooperation in this research.
Conflict of Interest Statement
The authors have no conflicts of interest in reporting.
Funding
The authors did not receive support from any organization for the submitted work.
References
- Watanabe, M., Chikuda, H., Fujiwara, Y., Furuya, T., Kanchiku, T., Nagoshi, N., ... & Taguchi, T. (2023). Japanese Orthopaedic Association (JOA) Clinical practice guidelines on the Management of Cervical Spondylotic Myelopathy, 2020–Secondary publication. Journal of Orthopaedic Science, 28(1), 1-45.
- Fehlings, M. G., Tetreault, L. A., Riew, K. D., Middleton, J. W., Aarabi, B., Arnold, P. M., ... & Wang, J. C. (2017). A clinical practice guideline for the management of patients with degenerative cervical myelopathy: recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression. Global spine journal, 7(3_suppl), 70S-83S.
- Friesen, A. C., Detombe, S. A., Doyle-Pettypiece, P., Ng, W.,Gurr, K., Bailey, C., ... & Duggal, N. (2024). Characterizing mJOA-defined post-surgical recovery patterns in patients with degenerative cervical myelopathy. World Neurosurgery: X, 21, 100267.
- Williams, J., D’Amore, P., Redlich, N., Darlow, M., Suwak, P., Sarkovich, S., & Bhandutia, A. K. (2022). Degenerative cervical myelopathy: evaluation and management. Orthopedic Clinics, 53(4), 509-521.
- Shigeo Ueda, Jiro Ohara, Atsuhiro Toyoshima et al. Current status and opinions for surgical treatment of cervical spondylotic myelopatht. Japanese Journal of Neurosurgery. 2023, 291-299. doi: 10.7887.
- Suzuki Yumi, Fujii Hiromi, Sato Yoshizumi, Hayashi Masahiro. Characteristics of grip and pinch strength in cervical spondylotic myelopathy, JJOT. 2011, 1479-1484 (in Japanese).
- Suzuki Yumi, Fujii Hiromi, Hayashi Masahiro. Comparison of thumb-index palmer pinch strength between 21 mm and 53 mm distance in the cervical myelopathy patients, 46th Japanese Occupational Therapy Congress and Expo. 2012; Miyazaki (in Japanese).
- Sato Yoshizumi, Suzuki Yumi, Fujii Hiromi, Hayashi Masahiro. Relations between ability to open a PET bottle cap and finger function in Cervical spondylotic myelopathy patients, JJOT. 2012, 415-420 (in Japanese).
- Suzuki Yumi, Fujii Hiromi, Hayashi Masahiro. Relationship among opening a small sack, pinch strength and finger spasticity in cervical spondylotic myelopathy, 47th Japanese Occupational Therapy Congress and Expo. 2013; Osaka (in Japanese).
- Suzuki Yumi, Hayashi Masahiro, Fujii Hiromi. Occupational therapy for cervical spondylotic myelopathy patient: Relation between upper extremity function and daily activities observed in one case. The Bulletin of Yamagata Occupational Therapists Society. 2014, 12(1), 18-27 (in Japanese with English abstract).
- Fujii Hiromi, Suzuki Yumi, Hayashi Masahiro. Characteristics of pinch strength recovery in cervical spondylotic myelopathy patients. The Bulletin of Yamagata Occupational Therapists Society. 2014, 12(1), 4-12 (in (Japanese with English abstract) and figure legends).
- Fujii Hiromi, Suzuki Yumi, Hayashi Masahiro. Recovery of pinch strength in cervical spondylotic myelopathy patients using bottle cap opening motion. Volume 6, 16th International Congress of the World Federation of Occupational Therapists (Yokohama). 2014.
- Ono, K., Ebara, S., Fuji, T. A. K. E. S. H. I., Yonenobu, K. A. Z. U. O., Fujiwara, K. E. I. J. U., & Yamashita, K. (1987). Myelopathy hand. New clinical signs of cervical cord damage. The Journal of Bone & Joint Surgery British Volume, 69(2), 215-219.
- Kanauchi, Y., Murase, T., Nishiwaki, M., Odagiri, M., Wanezaki, Y., & Ishikawa, H. (2023). Study of Reliability and Validity of the Load Cell-Type Hand Dynamometer Compared to the Jamar Dynamometer and the Number of Reliable Grip Strength Measurements. The Journal of Hand Surgery (Asian Pacific Volume), 28(05), 562-572.
- Demura, S., & Miyaguchi, K. (2009). Evaluation of muscle power exerted by explosive gripping. The Journal of Strength & Conditioning Research, 23(2), 465-471.
- Silva-Santos, T., Guerra, R. S., Valdiviesso, R., & Amaral, T. F. (2024). Hand Grip Force–Time Curve Indicators Evaluated by Dynamometer: A Systematic Review. Nutrients, 16(12), 1951.
- Kapandji, A. I., & Kapandji, I. A. (2007). The Physiology of the Joints: The Upper Limb. Volume One. Churchill Livingstone.
- Kamakura, N. (2022). Postures and Movement Patterns of the Human Hand: A Framework for Understanding Hand Activity for Clinicians and Engineers. Universal-Publishers.
- Lee, S. H., & Gong, H. S. (2020). Measurement and interpretation of handgrip strength for research on sarcopenia and osteoporosis. Journal of bone metabolism, 27(2), 85.
- Zhang, Y., Miyai, N., Abe, K., Utsumi, M., Uematsu, Y., Terada, K., ... & Arita, M. (2021). Muscle mass reduction, low muscle strength, and their combination are associated with arterial stiffness in community-dwelling elderly population: the Wakayama Study. Journal of Human Hypertension, 35(5), 446-454.
- Kubota, H., Demura, S., & Kawabata, H. (2012). Laterality and age-level differences between young women and elderly women in controlled force exertion (CFE). Archives of gerontology and geriatrics, 54(2), e68-e72.
- Nagai, K., Miyamato, T., Okamae, A., Tamaki, A., Fujioka, H., Wada, Y., ... & Domen, K. (2018). Physical activity combined with resistance training reduces symptoms of frailty in older adults: A randomized controlled trial. Archives of gerontology and geriatrics, 76, 41-47.
- Lee, H., & Lee, S. H. (2022). Effectiveness of multicomponent home-based rehabilitation in elderly patients after hip fracture surgery: a randomized controlled trial. Journal of Personalized Medicine, 12(4), 649.
- García-Hermoso, A., Huerta-Uribe, N., Izquierdo, M., González-Ruíz, K., Correa-Bautista, J. E., & Ramírez-Vélez, R. (2025). Comparative lipidomic profiling in adolescents with obesity and adolescents with type 1 diabetes. Current Problems in Cardiology, 102991.
- Joosten, E., Detroyer, E., & Milisen, K. (2016). Effect of anaemia on hand grip strength, walking speed, functionality and 1 year mortality in older hospitalized patients. BMC geriatrics, 16, 1-6.
- Bohannon, R. W. (2019). Grip strength: an indispensable biomarker for older adults. Clinical interventions in aging, 1681-1691.