Case Report - (2023) Volume 8, Issue 2
Extranodal Nk/T-Cell Lymphoma, Nasal Type: Clinical Cases Presentation and Review of Literature
Received Date: Jan 30, 2023 / Accepted Date: Feb 06, 2023 / Published Date: Feb 15, 2023
Abstract
Extranodal NK/T-cell lymphoma, nasal type (ENKTL-NT) is a rare form of non-Hodgkin’s malignant lymphoma, accounting for 1.4% of all lymphomas [1]. It is highly invasive and has a predilection for the nasal cavities, nasopharynx, and paranasal sinuses. It often affects middle-aged men and is strongly associated with Epstein- Barr virus (EBV). The incidence of ENKTL varies greatly from region to region, being highest in East Asia and Latin America where EBV infection in young children is widespread. We report two cases of extranodal NK/T-cell lymphoma of the nasal type diagnosed at a localized stage.
Keywords
NK/T-Cell Lymphoma, Ebv Infection, Oropharynx, Nasopharyngeal Carcinoma
Introduction
Extranodal NK/T-cell lymphoma, nasal type (ENKTL-NT) is a rare form of non-Hodgkin’s malignant lymphoma, accounting for 1.4% of all lymphomas [1]. It is highly invasive and has a predilection for the nasal cavities, nasopharynx, and paranasal sinuses. It often affects middle-aged men and is strongly associated with EpsteinBarr virus (EBV). The incidence of ENKTL varies greatly from region to region, being highest in East Asia and Latin America where EBV infection in young children is widespread. We report two cases of extranodal NK/T-cell lymphoma of the nasal type diagnosed at a localized stage.
Case Report
Case Report 1
comorbidities, presenting since June 2020 with bilateral nasal obstruction associated with frontal headaches and odynophagia. Symptoms worsened with the onset of dysphagia to both solids and liquids food. After a period of wandering around, the patient was referred to the university hospital for treatment. On admission, the examination of the oral cavity showed halitosis, a fetid whitish coating on the soft palate and oropharynx, and a furred tongue. The examination of the other organs was normal.
A computed tomography scan of the face showed a right posterolateral rhino-pharyngeal thickening suggesting a tumoral aspect. The biopsy of the cavum under local anesthesia showed a malignant round cell tumor, initially suggesting a lymphomatous process. Immunohistochemical study showed positivity of the tumor cells for CD3, CD56, EBV, weak positivity for CD30, and negativity for CD20 and CD5, with a Ki67 proliferation index of 80%. The diagnosis of NK/T-cell lymphoma was made.
The cervico-thoraco-abdomino-pelvic scan and PET-CT scan did not show any other locations. HIV and HBV-HCV serology were negative. The Epstein-Barr virus (EBV) was positive with a viral load of 2.49 log copies/ml. The lymphoma was classified as stage IB according to the Ann Arbor classification (Table 1).
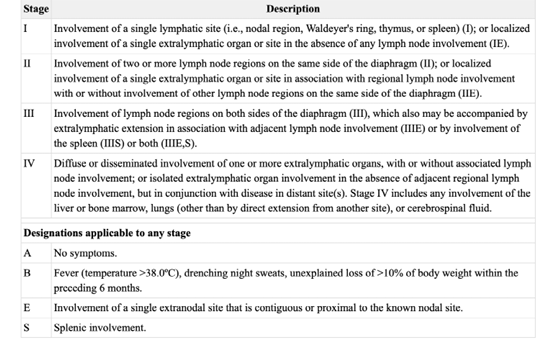
Table 1: Ann Arbor classification.
The patient received chemotherapy according to the MAD protocol (methotrexate-L-asparginase-dexamethasone). He then underwent locoregional radiotherapy at a dose of 50 Gy in 25 fractions (2Gy fractions/ ; 5 fractions/week).
For planning radiation treatment, we use CT simulator (Siemens, Erlangen, Germany).
The postchemotherapy gross tumor volume (GTV) was contoured in MRI and adjusted on the planning CT. For CTV, 5-mm margin was given around postchemotherapy GTV to have high-risk CTV (CTV-HR), and was adjusted on the planning CT to restricted natural barriers such as bone and air. CTV was expanded by isotropic 5 mm margin to generate planning target volume (PTV) and it also include the anatomic sites at the highest risk of tumour invasion surrounding the nasopharynx.
Our delineation was based on the International guideline for the delineation of the clinical target volumes (CTV) for nasopharyngeal carcinoma published by Anne W. Lee. The dose prescription was 50 Gy and 45 Gy.
OARs (cord, brainstem, optic chiasm, right eye, right lens, right retina, right optic nerve, temporal lobes, cochleae, right parotid gland, left parotid gland, oral cavity, larynx,) were contoured. Planning goals for the PTV based on ICRU 83 were the following: at least 90% and 95% of the prescribed total do (PTD) encompassing at least 98% and 95% of PTV, respectively (V≥98% and V≥95%, respectively); and no more than 2% of PTV received more than 107% of the PTV (V≤ 2%).
The following constraints were set for some OARs: for cord, the maximum dose received by 2% of its volume less than 45 Gy (D2%<45 Gy); for brainstem, D2%<55 Gy; for optic chiasm, D2%<60 Gy; for temporal lobes, D2%<65 Gy; for paritod gland Dmean<26 Gy et V30<43%, for oral cavity Dmean<30-40Gy, and lastly, the mean dose received by right cochleae and left cochleae was respectively Dmean 25Gy and 23Gy.
Two arcs volumetric modulated arc therapy (VMAT) plan with 6-MV photon beams was set by the medical physicist. VMAT plan was done with Elekta Versa HD. Patient position was verified weekly by kV cone beam CT imaging prior to treatment.
The patient tolerated the treatment and was seen weekly during treatment by our doctors. No significant side effects were observed except mucite and oesophagite grade 1.
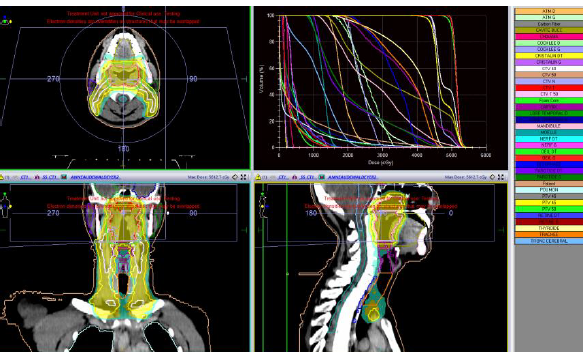
Figure 1: Computed tomography scan showing the target volumes CTV postchemotherapy in red: CTV-HR and PTV-HR in pink and green, respectively. (C) Volumetric modulated arc therapy was delivered to the region of high risk, to doses of 66 Gy (95% isodose line in orange). GTV, gross tumor volume; CTV, clinical target volume; PV, planning target volume; HR, high risk.
Currently, the patient is in complete clinical and radiologic remission after a follow-up of 27 months.
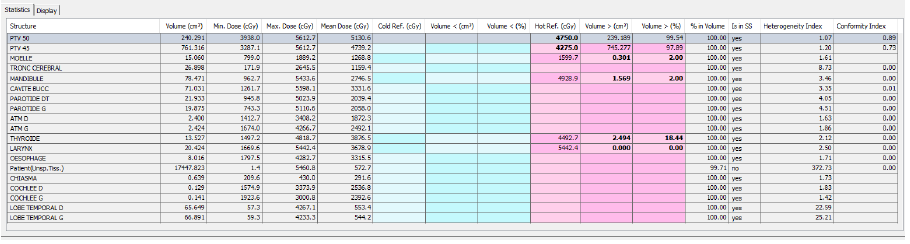
Figure 2: Dose-volume histogram distribution of the following structures: planning target volume (green), chiasma (Pink), left temporal
lobe (dark blue), right temporal lobe (dark green), spinal cord (green, pickle), brainstem (blue sky), right parotid(purple), oral cavity
navy green.
Case Report 2
A 45-year-old patient has been experiencing dysphonia and odynophagia for one year. These symptoms have been ignored by the patient until they worsened to total dysphagia and dyspnea in the context of a significant deterioration of their general health, which led the patient to seek treatment at the university hospital.
Figure 3: Axial CT of laryngeal tumor.a
On December 21st, 2019, a laryngoscopy was performed and revealed a process that affected the entire left vocal cord, extending to the right vocal cord, accompanied by mucosal oedema. Two deep biopsies, along with IHC study were used to diagnose an Extranodal NK/T-cell lymphoma in the larynx.
The patient underwent poly-chemotherapy treatment according to the MAD protocol (methotrexate, L-asparaginase, dexamethasone). Immediately, after the first round of treatment, the patient developed acute pancreatitis stage E, due to to the L-asparaginase. The chemotherapy protocol was then changed to the DeVIC protocol (dexamethasone, etoposide, ifosfamide, carboplatin). Afterwards, the patient received external loco-regional radiotherapy at a dose of 50 Gy in 25 fractions, using the VMAT technique (Figure 4). The treatment resulted in a complete metabolic remission.
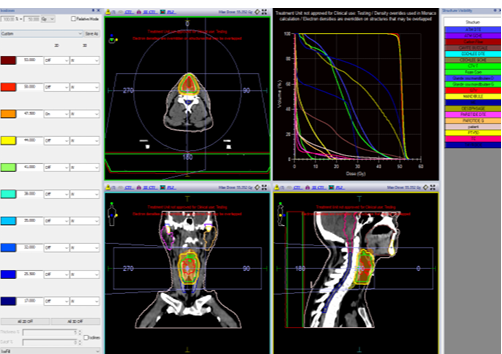
Figure 4: Computed tomography scan showing the target volumes: postchemotherapy GTV in red, CTV-HR and PTV-HR in green and yellow, respectively. (C) Volumetric modulated arc therapy was delivered to the region of high risk, to doses of 66 Gy (95% isodose line in orange). GTV, gross tumor volume; CTV, clinical target volume; PV, planning target volume; HR, high risk.
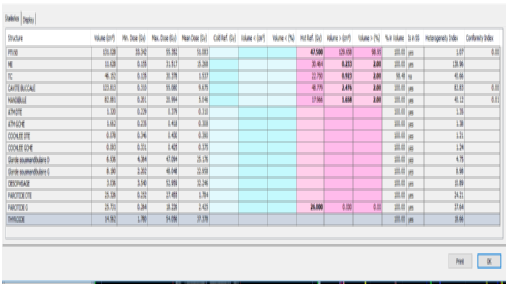
Figure 5: Dose-volume histogram distribution of the following structures: planning target volume (yellow), spinal cord (bleu), brainstem (Magenta), right parotid(pink), left parotid (orange), oral cavity (brown).
Dose-volume histogram distribution of the following structures: planning target volume (light orange), right parotide (pink), left parotid (orange) spinal cord (green), brainstem (red), oral cavity (turquois), mandibule (yellow), oesophage (navy green), right sub mandibular gland (bleu), , thyroide (dark blue).
Planning goals for the PTV based on ICRU 83 were the following: at least 90% and 95% of the prescribed total do (PTD) encompassing at least 98% and 95% of PTV, respectively (V≥98% and V≥95%, respectively); and no more than 2% of PTV received more than 107% of the PTV (V≤2%).
The following constraints were set for some OARs: for cord, the maximum dose received by 2% of its volume less than 45 Gy (D2%<45 Gy); for brainstem, D2%<55 Gy; for optic chiasma, D2%<60 Gy; for paritod gland Dmean<26 Gy et V30<43%, for oral cavity Dmean<30-40Gy; for the mandibule Dmean≤70 Gy et Dmax<60Gy, lastly, the mean dose received by the right cochleae and left cochlea was less than (Dmean<45Gy).
One arc volumetric modulated arc therapy (VMAT) plan with 6-MV photon beams was set by the medical physicist. VMAT plan was done with Elekta Versa HD. Patient position was verified weekly by kV cone beam CT imaging prior to treatment. The patient tolerated the treatment and was seen weekly during treatment by our doctors. No significant side effects were observed except mucite and oesophagite grade 1.
However, the patient passed away one year later following a macrophagic activation syndrome, which led to sepsis and failure of multiple internal organs.
Discussion
Nasal type extranodal natural killer/T-cell lymphoma (ENKTL) is a rare and malignant form of non-Hodgkin lymphoma (NHL) that arises from natural killer (NK) cells and cytotoxic T lymphocytes. The etiology of this subtype of NHL remains unclear, however, a strong association with Epstein-Barr virus (EBV) has been established in literature [2-4]. The most commonly affected extranodal sites in ENKTL are the nose, cavum, and paranasal sinuses, which is observed in roughly 70% of cases [5,6].
cThe demographic primarily affected by this subtype of NHL is young adult males, as observed in the present case series.
Despite treatment, the prognosis for ENKTL remains poor due to the high incidence of local recurrences and the development of macrophagic activation syndrome (MAS), which is a feared complication that results in systemic symptoms such as fever and weight loss. MAS occurs in 8-13% of cases, as observed in the present patient [7]. ENKTL is characterized by clinical polymorphism, which can contribute to diagnostic difficulties and delayed therapeutic intervention. Symptoms of ENKTL are often non-specific and primarily consist of facial edema, nasal obstruction, and epistaxis.
Diagnosis and assessment of disease extent are primarily based on a comprehensive clinical examination, nasal endoscopy, MRI of the skull and face, and thoraco-abdominal scanning. Positron emission tomography (PET) scanning is routinely performed to evaluate for systemic involvement and to search for locoregional extension due to the high uptake of FDG.
Obtaining a biopsy specimen enables histological examination, which will be consistently complemented by immunohistochemical analysis. This analysis typically reveals expression of CD2 antigen, CD56, and cytotoxic molecules such as TIA-1, perforin, and granzyme B. The expression of CD3 is variable, while CD5, CD4, and CD8 are typically negative [8]. Detection of EpsteinBarr virus in biopsy specimens is a key diagnostic criterion per the World Health Organization (WHO) classification, as well as the presence of cytotoxic granules [9]. In the present case, the EBV positivity was established via IHC analysis.
Computed tomography (CT) scanning is a fundamental diagnostic tool for T/NK lymphomas as it allows for lesion assessment and evaluation of bone and sinus involvement of the base of the skull, as well as pre-treatment assessment [10].
Magnetic resonance imaging (MRI) is superior in the evaluation of soft tissue involvement and cerebrospinal structure invasion.
The two patients underwent a facial CT scanner completed by MRI for the first patient and revealing a right posterolateral rhinopharyngeal thickening extended to the oropharynx in the first patient and involvement of both vocal cords with bilateral cervical lymphadenopathy in the second patient.
The treatment of T/NK cell lymphomas is primarily based on the Ann Arbor classification. For localized stages, radiation therapy at doses of at least 52Gy is the primary treatment modality, resulting in complete remission in up to 80% of cases and a five-year overall survival rate ranging from 40 to 59% [12]. For advanced stages (III and IV), aggressive chemotherapy is the primary treatment option, resulting in complete response in less than 15% of cases. [13].
Some teams propose the use of anthracycline-based polychemotherapy followed by external radiation therapy consolidation for patients less than 60 years old, and the same protocol without anthracyclines for patients over 60 years old [14]. In case of non-response or early relapse, alternative chemotherapy protocols such as 2nd or 3rd generation polychemotherapy (ranimustine, etoposide, carboplatin, and cyclophosphamide) may be used, along with bone marrow autograft reinjection when necessary.
Despite therapeutic advances, T/NK cell lymphomas remain poor prognosis tumors, with a five-year overall survival rate varying between 10 and 45% depending on the series [15,16].
The aggressive therapy required for this type of lymphoma can also lead to significant side effects. Despite recent advances in the treatment of NK/T-cell lymphomas, the prognosis remains poor and further research is needed to improve the outcome of these patients.
Conclusion
Nasal NK/T-cell lymphoma, a rare form of lymphoma, is primarily identified through immunohistochemical analysis. The standard treatment for localized stages involves a combination of chemotherapy and radiation therapy. However, the toxicity associated with these treatments presents a challenge for patients. Further research is needed to establish more effective and tolerable treatment options for individuals with localized nasal ENKTL.
Conflict of Interest Statement
The authors declare no conflict of interest.
References
1.Kwong YL (2011) The diagnosis and management of extranodal NK/T- cell lymphoma, nasal-type and aggressive NK-cell leukemia. J Clin Exp Hematop 51(1):21-28.
2. Forcioli J, Meyer B, Fabiani B (2005) Granulome malin centrofacial ou lymphome nasal T/NK EMC Oto-Rhino. Laryngologie 390.
3. Hmidi M, Kettani M, Elboukhari A, Touiheme N, Messary A (2003) Lymphome T/NK nasosinusien. Ann Fr Otolaryng Chir Cervico- fac 130:149-152.
4. Gru AA, Haverkos BH, Freud AG, Hastings J, Nowacki NB, et al. (2015) The Epstein-Barr virus (EBV) in T cell and NK cell lymphomas: time for a reassessment. Curr Hematol Malig Rep 10:456-467.
5. Tababi S, Kharrat S, Sellami M, Mamy J, Zainine R, et al. (2012) Extranodal NK/T-cell lymphoma, nasal type: report of 15 cases. Eur Ann Otorhinolaryngol Head Neck Dis 129(3):141-147.
6. Jimnez-Prez JC, Yoon MK (2017) Natural Killer T-Cell Lymphoma of the Orbit: an evidence-based approach. Semin Ophthalmol 32(1):116-124.
7. Al-Hakeem DA, Fedele S, Carlos R, et al. (2007) Extranodal NK/T-cell lymphoma, nasal type. Oral Oncol 43:4-414.
8. Forcioli J, Meyer B, Fabiani B (2005) Granulome malin centrofacial ou lymphome nasal T/NK. Encycl Med Chirurg Oto-Rhino-Laryngologie 2:390.
9. Chan JKC, Quintanilla-Martinez L, Ferry JA, Peh SC (2008) Extranodal NK/T-cell lym-phoma, nasal type. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, editors. World Health Organization Classification of Tumours, WHO Classifica- tion of Tumours of Haematopoietic and Lymphoid Tissues. 4th ed. Lyon, France: International Agency for Research on Cancer (IARC); 285-288.
10. Kharoubi S (2005) Tumeurs malignes des fosses nasales aÌ? propos de 21 cas. Cancer Radiother 9:187-195.
11. Mestiri S, Zeglaoui I, Sriha B, et al. (2008) Extra-nodal T, lymphomas of the nasal cavities and sinuses. Ann Otolaryngol Chir Cervicofac 125:188-192.
12. You JY, Chi KH, Yang MH, et al. (2004) Radiation therapy versus che- motherapy as initial treatment for localized nasal natural killer (NK)/T-cell lymphoma: a single institute survey in Taiwan. Ann Oncol 15:618-625.
13. Kwong YL (2005) Natural killer-cell malignancies: diagnosis and treat-ment. Leukemia 19:2186-2194.
14. Ribrag V, Ell Hajj M, Janot F, Girinsky T, Domenge C, et al. (2001) Early locoregional high-dose radiotherapy is associated with long-term disease control in localized primary angiocentric lymphoma of the nose and nasopharynx. Leukemia 15(7):1123-1126.
15. Armitage JO (2009) Peripheral T-cell lymphomas: their time has come. Oncology (Williston Park) 23:1151-1152.
16. Lee J, Park YH, Kim WS, et al. (2005) Extranodal nasal type NK/T- cell lymphoma: elucidating clinical prognostic factors for risk-based stratification of therapy. Eur J Cancer 41:14021408.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



