Case Report - (2022) Volume 7, Issue 6
Extended pedicle subtraction osteotomy in combination with novel four-rod technique in an ankylosing spondylitis patient with neglected thoracolumbar fracture: a case report
Received Date: May 31, 2022 / Accepted Date: Jun 06, 2022 / Published Date: Jun 15, 2022
Abstract
Introduction: Ankylosing spondylitis is an autoimune disorder that affects mainly the enthesis of the spinal ligaments and capsules and causes a progressive fusing of the vertebra bodies. The ankylosed spine will lose the ability of absorbing and dissipating the axial loading force and therefore becomes vulnerable with injuries.
Case report: We report a 27-year-old male patient with past history of ankylosing spondylitis who suffered from a neglected thoracolumbar fracture after a traffic accident one year before admission. He noticed an ongoing kyphotic deformity over time to the point that he could not have a horizontal gaze at present. The full spine Xray depicted a severe kyphosis at L1/2 (80o ) due to a nonunion L1/2 flexion-distraction fracture. There were no neurological deficits at admission.
Surgical treatment and outcome: The patient underwent an extended L2 pedicle subtraction osteotomy and long instrumentation from T10 to L5. The clinical and radiological outcome were satisfactory as the global kyphosis was reduced from 80o to 20o and patient could regain his normal upright posture, even better than before the accident.
Conclusion: Kyphotic deformity in ankylosing spondylitis patients, especially with traumatic causes is always a challenge for spinal surgeons as corrective surgeries involve potential neurological complications. Conventional pedicle subtraction osteotomy remains a procedure of choice. The downside of this technique is the relatively high risk of non-union and implant failure which can be improved by reinforcing two additional short rods to the whole configuration.
Introduction
Ankylosing spondylitis (AS) is an autoimmune disease that mainly affects the enthesis of ligaments and joint capsules of the spine, causing gradual ossification of these structure, and as consequence the vertebrae become fused together from pelvis to cervical region [2,13-16].
The disease is more common among men (male/female ratio ranging from 5/1 to 9/1) [2], with an onset age between the second and fourth decades [2]. While the pathogenesis remains unclear, HLA B27 factor (90% of AS patients are HLA B27 positive) [2], inflammatory cellular infiltrates, genetic and environmental factors that trigger autoimmune response are thought to have key roles [2,16]. In early stage, patients usually have back stiffness and pain in the morning. As the disease progresses, back pain will decrease in intensity and so does the mobility of the spine due to ongoing ossification. Eventually, when all ligaments, discs and facet joints are completely fused, the range of motion of the spine is totally lost in all three planes. One hallmark of the latter stage of AS is progressive kyphotic deformity, which is thought to be associated with osteoporosis and wedging deformity of the vertebral bodies [15].
Surgical treatment is usually indicated when the kyphosis causes severe changes in sagittal balance and affects the quality of life of AS patients [8]. Another indication of surgery is fractures in those patients as the fused spine will have the bone healing similar to long bone with high risk of delayed or non-union with conservative treatment, not to mention the risk of late onset neurological deficits due to kyphotic deformity [9]. When dealing with severe kyphotic deformity in AS patients, pedicle subtraction osteotomy with its derivations is currently considered as the treatment of choice since it allows to adjust 25o to 45o of the kyphosis in one procedure [3,5,8].
In this paper, we report the case of a male ankylosing spondylitis patient with neglected lumbar fracture admitted due to severe 80o kyphosis. We described our novel pedicle subtraction osteotomy technique using 4 rods that was successfully applied on this case.
Case Report
History and Examination
It was a 27-year-old man admitted to our hospital due to severe kyphosis in the thoracolumbar spine and was unable to stand upright. One year before admission, the patient was injured in a traffic accident and started to experience symptoms including low back pain and lumbar kyphosis, which gradually progressed to the extent that dramatically limited work and daily activities. The patient has a history of ankylosing spondylitis diagnosed 10 years ago without any specific treatments.
Physical examination revealed severe kyphotic deformity at the thoracolumbar junction and a complete loss of range of motion of the entire spine (figure 1). Sensory-motor and sphincter activity remained within normal limits.
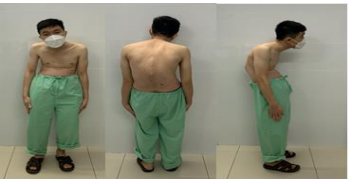
Figure 1: Preoperative appearance of patient. Note that the kyphosis at the thoracolumbar spine caused severe global sagittal imbalance with difficulty to maintain horizontal gaze.
Investigations
The findings of non-union of the anterior column can be observed at the L1-2 level, with the image of a neglected L1-2 flexiondistraction fracture on lumbar CT scans (figure 2a). The posterior column was bilaterally fused at L1-2 facet joints on CT scan (figure 2b). The full spine Xray showed severe kyphosis with apex at L1-2 discal space. The regional kyphotic angle (T10-L2) was 80o , with severe sagittal imbalance (SVA was 161 mm, PT was 46o , PI/LL mismatch was 31o ) (figure 3). The sagittal T2 MRI depicted the spinal cord is relatively compressed and tethered at the kyphotic apex but the signal of the conus medullaris is still within normal limits (figure 4).
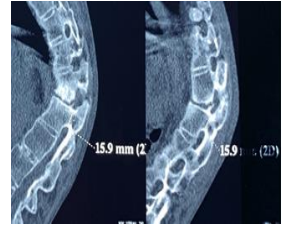
Figure 2: Findings of non-union of the anterior column at L1/2 disc space (a) and fused L1/2 facet joints in dislocated position (b).

Figure 3: Preoperative full spine Xray of patient. The T10-L2 kyphosis was 80o with severe sagittal imbalance: SVA was161 mm, PT was 46o , PI/LL mismatch was 31o
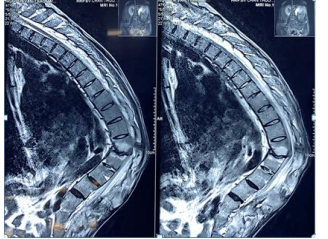
Figure 4: Severe kyphosis at L1/2 discal space causing spinal cord tethering depicted on T2-weighed sagittal MRI. However, the T2 signal of the conus medullaris was still normal.
Surgical Treatment and Outcome
Surgical Planning
We acknowledge the difficulties of this case, given the severe kyphosis and normal neurological status outcome of our patients and therefore, careful surgical planning with different alternative scenarios was done.
The full spine Xray was analysed by the software Surgimap, where simulative surgery could be done in terms of position of cutting lines and angle of osteotomy and projective postop image of the spine with new sagittal balance parameters was built (figure 5 a and b).
Then, a multidisciplinary discussion has been organized with the participation of spine, neurology, anesthesiologist and rehabilitation experts. The technique of choice was an extended pedicle substraction osteotomy (grade 4 osteotomy) stabilized by a novel four-rod technique.
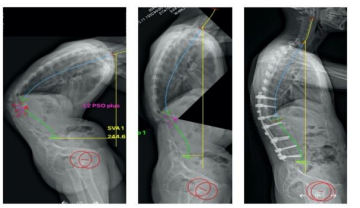
Figure 5: Preoperative full spine Xray (a), simulated Xray created by Surgimap software (b) and postoperative full spine Xray (c). Note that the simulated Xray had high accuracy and was very close to reality.
Operative Technique
The patient was intubated for general anesthesia and positioned prone on the operating table which was bent in flexion in order to adapt to the shape of his kyphotic spine. Pressure points (chest, anterior superior iliac spine, knee, ankle) were carefully padded (figure 6). Midline incision was made to expose the posterior arch and the facet joints of the vertebrae T10 to L5. We located the entry points to insert the pedicle screws from T10 to L1 and from L3 to L5, and then check the direction of the pedicle with C-arm. We inserted screws from vertebra T10 to L1 and from L3 to L5. The L2 vertebra was not instrumented because the pedicles will be removed during osteotomy. We placed 2 short rods from L1 to L3, crossing the L2 vertebrae. The entire L2 superior endplate and the fibrotic tissue at L1/2 discal space were removed in the way of extended pedicle subtraction osteotomy technique. We then gently adjusted the operating table back to normal position for reduction purpose, while bilaterally applying compressive force on the screw heads at L1 and L3 vertebra to close the V-shaped osteotomy space (figure 7a). During kyphosis correction, spinal cord function is monitored using motor evoked potential (MEP) system, should any changes in the neurological signals occurred, the procedure would be stopped. Finally, 2 long rods were bent with respect to the final shape of the spine from T10 to L5 (figure 7b) and bypass the L1 and L3 screws which already connected to the short rods. Posterolateral grafting was performed with autologous bone harvested from the lamina and the resected part of the L2 vertebral body. Two rod connectors were inserted caudally and rostrally to reinforce the whole configuration. The incision was then closed layer by layer. The whole operation took 5 hours from skin to skin with 1500 ml of blood loss. There were no neurological complications after the operation.
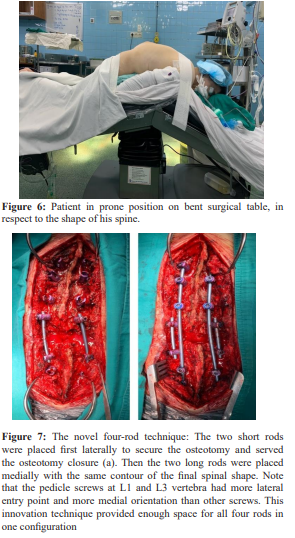

Figure 8: Body shape and sagittal balance of patient before (a) and after surgery (b). Note that after the operation, patient could maintain his horizontal gaze without difficulties
Postoperative Course
Drainage system and urinary catheter were removed 24 hours postsurgery. Prophylactic intravenous antibiotic was prescribed during the first 3 days. The patient was able to leave the bed since day 3 with long thoracolumbar brace. The body shape of the patient was dramatically corrected as the overall sagittal balance of the entire body was restored (figure 8). He was discharged after 7 days when VAS index was below 3.
Postoperative Radiological Images
The postop full spine Xray revealed a remarkable kyphotic correction, with the kyphotic degree plummeted from 80o to 21o and all sagittal balance parameters was greatly improved, to almost ideal values (figure 9). To be specific, the SVA changed from 80o to 21o , PT decreased from 46o to 29o , PI/LL mismatch decreased 31o from to 17o .
At 6 months post-operation, callus formation was already visible on X-ray (figure 10).

Figure 9: Comparison between preoperative and postoperative full spine xrays on AP view (a) and sagittal view (b). The T10-L2 kyphosis was reducing from 80o to 21o and all sagittal parameters returned to acceptable values.
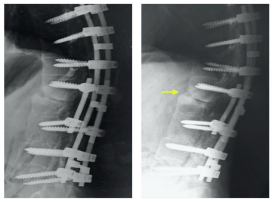
Figure 10: Xray of the osteotomy on day 5 postop (a) and sixmonth follow-up (b). Note that callus formation could be seen at six-month follow-up (yellow arrow)
Discussion
According to the literature, neglected fractures in AS patients are not rare as initial fracture lines are not easy to detect on plain Xray. However, not many cases were reported with severe kyphosis and normal neurological status similar to our case. This could be explained by the fact that both L1/2 facet joints were fused and stopped the deformity to a limit where the spinal cord still well tolerated. The normal neurological status aggravated the difficulty level of the surgery, as the surgeons must ensure that there would be no iatrogenic neurological complication throughout the procedure. Facing such adversities, careful and detailed planning was carried out with the support of Surgimap software. Preoperative images were measured and analyzed to provide a plan for osteotomy and the virtual corrective maneuver were simulated by the software. The final surgical outcome showed that prediction from the software was accurate (figure 5b and c) and helped to restore the spine to a nearly perfect shape. This confirmed the accuracy of Surgimap, which was in line with other studies [1,10-12].
According to previous studies, the healing time for this technique can be up to two years, and if the instrument is not strong enough, the risk of implant failure is relatively high and could affect the entire treatment outcome [4]. There were some reports of implant failure and nonunion when using conventional PSO with only two rods [4], and some authors recommended extra rods should be added to the instrumentation for reinforcement purpose [6]. Dualheaded screws (can be connected with two rods at the same time) [7] and connectors [4] are commonly used to facilitate the insertion of four rods in just one configuration. The main disadvantage of this method is the high cost of instrument, not to mention the unavailability of those specialized screws and connectors in our country.
Given these reasons, the need to improve the technique with the goal of putting two more rods to the main configuration using conventional instruments is imperative, since a large proportion of operated AS patients belongs to the low-income class. Our improvements are as follows: instead of placing two main rods on both sides from the beginning, we firstly put two short rods on the screws of L1 and L3 vertebrae both sides (the upper and lower segments to the osteotomed L2 vertebra). Then, instead of multiple time of removing the rods, readjusting the contour of the rods and putting them back to the screw heads, we can shorten the procedure with the two short rods by just compressing on the screw heads of the upper and lower vertebra of the osteotomy level (in our case, the L1 and L3 screws). Because the short rods connect only the L1 and L3 screws on both sides, it is unnecessary to reshape these short rods during the reduction process. During the whole osteotomy procedure, the short rods played a crucial role when helping the gap closure as well as preventing translation and sub-luxation of the two spinal portions. Finally, when the osteotomy closure was finished, the surgeon just had to bend the two main rods one time only in respect to the final shape of the spine. To facilitate the insertion of all four rods, we have chosen on purpose the entry points of the four screws at L1 and L3 more lateral than conventional technique, and then oriented those screws more medially than usual. As a result, the two short rods would stay outside and wouldn’t interfere with the trajectory of the two long rods (figure 7b). Normal poly-axial screws were used to facilitate the rod insertions. The efficacity of our innovative technique could be demonstrated on plain Xray with clear callus formation after 6 months.
Conclusion
This case is technically challenging from all aspects as the degree of kyphosis is high and the neurological status of our patient was still intact. Thorough consultation, careful surgical planning played an important role in the success of this surgery. The novel four-rod technique in combination with pedicle subtraction osteotomy could provide adequate stability necessary for good clinical outcome and bone healing.
References
1. Akbar M, Terran J, Ames CP, Lafage V, Schwab F (2013) Use of Surgimap Spine in sagittal plane analysis, osteotomy planning, and correction calculation. Neurosurg Clin N Am 24(2):163-172.
2. Bond (2013) Ankylosing spondylitis: diagnosis and management. Nurs Stand 28(16-18):52-9.
3. Bridwell KH, Lewis SJ, Rinella A, Lenke LG, Baldus C (2004) Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical technique. J Bone Joint Surg Am 86:44-50.
4. Dickson DD, Lenke LG, Bridwell KH, Koester LA (2014) Risk factors for and assessment of symptomatic pseudarthrosis after lumbar pedicle subtraction osteotomy in adult spinal deformity. Spine (Phila Pa 1976) 39(15):1190-1195.
5. Diebo B, Liu S, Lafage V, Schwab F (2014) Osteotomies in the treatment of spinal deformities: indications, classification, and surgical planning. Eur J Orthop Surg Traumatol 24:S11- 20.
6. Gupta S, Eksi MS, Ames CP, Deviren V, Durbin-Johnson B, et al. (2018) A Novel 4-Rod Technique Offers Potential to Reduce Rod Breakage and Pseudarthrosis in Pedicle Subtraction Osteotomies for Adult Spinal Deformity Correction. Oper Neurosurg (Hagerstown) 14(4):449-456.
7. Jakub Godzik (2021) Impact of dual-headed pedicle screws on the biomechanics of lumbosacral junction multirod constructs. J eurosurg Spine 19(9):S67.
8. Koller H, Koller J, Mayer M, Hempfing A, Hitzl W (2018) Osteotomies in ankylosing spondylitis: where, how many, and how much?. Eur Spine J 27(Suppl 1):70-100.
9. Kurucan, Bernstein, Mesfin (2018) Surgical management of spinal fractures in ankylosing spondylitis. J Spine Surg 4(3):501-508.
10. Lafage R, Ferrero E, Henry JK, Challier V, Diebo B (2015) Validation of a new computer-assisted tool to measure spinopelvic parameters. Spine J 15(12):2493-2502.
11. 11.Langella F, Villafañe JH, Damilano M, Cecchinato R, Pejrona M (2017) Predictive Accuracy of Surgimap Surgical Planning for Sagittal Imbalance: A Cohort Study. Spine (Phila Pa 1976) 42(22):E1297-E1304.
12. Michael Akbar (2013) Use of Surgimap Spine in Sagittal Plane Analysis, Osteotomy Planning, and Correction Calculation. Neurosurg Clin N Am 24.
13. Pedersen, Maksymowych (2019) The Pathogenesis of Ankylosing Spondylitis: an Update. Curr Rheumatol Rep 21(10):58.
14. Smith (2015) Update on ankylosing spondylitis: current concepts in pathogenesis. Curr Allergy Asthma Rep 15(1):489.
15. Vosse D, van der Heijde D, Landewé R, Geusens P, Mielants H (2006) Determinants of hyperkyphosis in patients with ankylosing spondylitis. Ann Rheum Dis 65(6):770-774.
16. Zhu W, He X, Cheng K, Zhang L, Chen D (2019) Ankylosing spondylitis: etiology, pathogenesis, and treatments. Bone Res 7:22.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



