Research Article - (2024) Volume 1, Issue 1
Enhancing Reliability and Efficiency: An ASHRAE Level 2 Energy Audit of a Regional Hospital
2Assistant Professor, Department of Mechanical-Mechatronics Engineering. The LNM Institute Informati, India
Received Date: Jul 01, 2024 / Accepted Date: Jul 26, 2024 / Published Date: Aug 02, 2024
Copyright: ©2024 Vibhu Sharma, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Sharma, V., Unune, D. (2024). Enhancing Reliability and Efficiency: An ASHRAE Level 2 Energy Audit of a Regional Hospital. J Data Analytic Eng Decision Making, 1(1), 1-8.
Abstract
This study investigates the energy profile of a regional hospital in North America using an ASHRAE Level 2 Energy Audit. The audit aimed to assess the efficiency of existing systems, identify areas for improvement, and recommend cost-effective measures to reduce energy consumption and environmental impact. The analysis revealed a well-maintained heating system with efficient boilers. However, a critical concern emerged regarding operational risks due to the lack of redundancy in the cooling system. To address this vulnerability, the study recommends installing an air-cooled chiller for increased operational resilience. The economic feasibility of proposed improvements was evaluated, highlighting the balance between initial investment and long- term savings in energy costs and reduced greenhouse gas emissions. The findings contribute to the discourse on sustainable healthcare practices, emphasizing the importance of energy audits, strategic planning, and redundancy measures for optimized performance and environmental responsibility in hospitals.
Introduction
Efficient energy management is imperative for large institutions, particularly in sectors like healthcare where constant demand for power and precise climate control is essential for patient care and safety. Hospitals, in particular, are among the most energy-intensive facilities, operating 24/7 and requiring sophisticated energy systems to support their diverse operations. The implementation of advanced monitoring systems, infrastructure updates with energy-efficient materials, and regular energy audits are critical strategies employed to reduce energy usage and manage costs in these settings [1]. Healthcare facilities not only face substantial f inancial implications associated with energy consumption but also contribute significantly to environmental footprints due to their continuous and intensive energy use.
Amid growing concerns about climate change and rising energy costs, there is an increasing emphasis on improving energy efficiency and sustainability in healthcare infrastructure. This study delves into the energy profile of a regional hospital located in North America, utilizing data from calendar year 2020 to explore energy efficiency within the healthcare industry. Constructed in 2016, the hospital serves as a hub for a wide array of medical services and has been designed with modern energy conservation measures to support its around-the-clock operations. Despite the incorporation of best practice equipment and technologies, the dynamic nature of healthcare operations necessitates ongoing scrutiny and optimization to ensure sustained efficiency. This is particularly relevant given the evolving regulatory landscape and the imperative for healthcare institutions to reduce operational costs while maintaining high standards of patient care.
To address these challenges, the study undertakes an ASHRAE Level 2 Energy Audit, providing a comprehensive examination of the hospital’s energy systems. The objectives of the audit encompass evaluating both the performance and efficiency of existing systems, identifying potential areas for improvement, and exploring cost-effective measures that can contribute to energy savings and reduction of the facility & carbon footprint. Furthermore, the study aims to examine the critical balance between maintaining reliable patient care services and the pursuit of sustainability goals within the healthcare sector. In framing the audit & findings and their implications, the introduction sets the context for a holistic analysis of energy use within the hospital. By elucidating the complexities of managing a hospital & energy footprint and highlighting key strategies for optimization, the research aims to contribute to the broader discourse on sustainable practices in healthcare infrastructure. Through data-driven insights and practical recommendations for energy management, the study seeks to provide guidance for future planning and design of healthcare facilities, ultimately advancing efforts towards a more sustainable healthcare sector.
Literature Review
Healthcare facilities are crucial to society, offering indispensable services that demand consistent operational excellence and reliability. Hospitals, in particular, are among the most energy demanding facilities due to their continuous operations, strict environmental control requirements, and essential services. This review delves into the importance of comprehensive energy audits in hospitals, focusing on their role in boosting operational efficiency and environmental sustainability. The review draws on a broad range of research to detail the significant benefits and challenges of conducting these audits in healthcare settings. Hospitals have distinctive energy consumption patterns that greatly differ from other types of buildings. For example, they consume significantly more energy per square foot compared to typical commercial buildings [2]. This increased energy usage is largely due to the requirements for advanced medical equipment, extensive heating, ventilation, and air conditioning (HVAC) systems for infection control, and continuous lighting systems.
Energy audits are crucial for assessing energy use within a facility and identifying ways to enhance efficiency and cut costs. A comprehensive energy audit goes beyond merely recognizing patterns of energy use to provide insights into equipment performance and operational efficiencies [3]. This level of analysis is especially vital in hospitals where small improvements can lead to substantial cost savings and reductions in energy use. Numerous studies have underscored the effectiveness of Level 2 energy audits in identifying substantial energy savings in hospitals. These savings often come from upgrades to HVAC systems, optimized lighting, and more efficient use of medical equipment [4]. Furthermore, energy audits have been noted to significantly improve system reliability, an essential aspect in healthcare settings where power reliability directly affects patient safety and care quality. Improvements can include better emergency power systems, energy distribution, and planning for redundancy [5]. Implementing recommendations from energy audits can result in considerable cost savings, which is particularly beneficial for hospitals with tight budgets. These audits can expose inefficient practices and equipment, leading to immediate and sustained f inancial savings.
Energy conservation is also a key element of environmental sustainability. By lowering energy use, hospitals can reduce their carbon emissions, contributing to broader environmental goals. This is increasingly important as organizations face growing public and regulatory pressure to demonstrate environmental responsibility. Additionally, enhancements in energy systems can improve the indoor environment quality of hospitals, which can lead to better patient outcomes and increased staff productivity and satisfaction. Improved air quality, appropriate lighting, and optimal temperature control are known to decrease recovery times and boost staff satisfaction [6]. Energy efficiency improvements can assist healthcare facilities in meeting regulatory demands and achieving standards required for certain certifications, enhancing their reputation. Compliance with energy standards can also qualify hospitals for government incentives or rebates, further reducing the costs of implementing energy-efficient technologies [6].
Despite these benefits, the implementation of comprehensive energy audits presents challenges, including the initial costs, potential disruptions to hospital operations, and technical difficulties in retrofitting older systems with new technologies. However, these challenges can be mitigated through careful planning and phased implementation. Securing stakeholder support through clear communication about the benefits of energy audits is crucial for success. Additionally, training staff on new technologies and processes is essential to ensure the long-term benefits and maintenance of energy savings [3]. In a context of rising energy costs and increasing environmental consciousness, proactive energy management is becoming a strategic imperative for hospitals. Comprehensive energy audits, in particular, are pivotal, offering a roadmap for significant cost savings, operational improvements, and environmental benefits. This literature review emphasizes the crucial role of conducting these audits in hospitals, highlighting the immediate and long-term advantages, making them indispensable tools for modern healthcare facilities aiming to balance operational efficiency with environmental sustainability.
Methodology
Efficient energy management in healthcare facilities necessitates a systematic approach to auditing energy usage and identifying opportunities for improvement. This study follows the guidelines outlined by the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) for conducting a Level 2 Energy Audit, ensuring a comprehensive assessment of the regional hospital's energy systems and usage patterns.
Data Collection
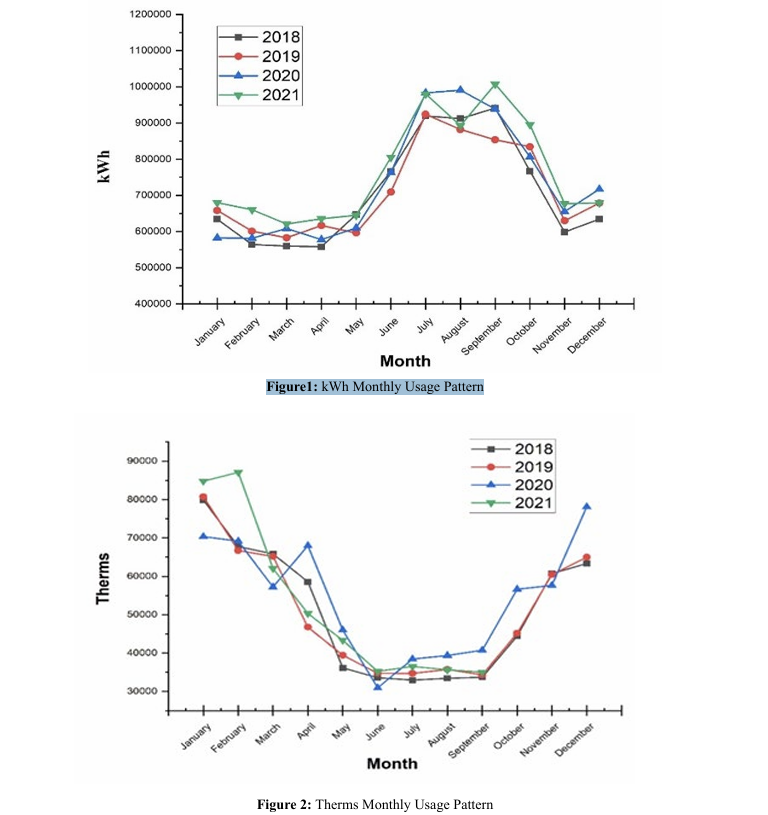
The audit commenced with an exhaustive collection of data pertaining to the hospital's energy infrastructure. This encompassed detailed inventorying of major energy-consuming systems, including heating, ventilation, and air conditioning (HVAC) equipment, lighting fixtures, and specialized medical devices. Monthly usage patterns for gas and electricity were meticulously recorded and analyzed, providing valuable insights into seasonal variations and consumption trends. Figures 1 and 2 depict the monthly usage patterns for electricity and gas, respectively, aiding in visualizing the fluctuations in energy demand over time. Additionally, pertinent information such as equipment type, capacity, age, and efficiency ratings were documented to establish a baseline understanding of energy consumption [7].
Historical Analysis
A thorough evaluation of the hospital's energy bills and consumption records spanning a significant period was conducted to discern patterns and fluctuations in energy demand. This historical analysis facilitated the identification of peak usage periods, enabling a deeper understanding of the factors influencing energy consumption. By scrutinizing historical data, the audit team gained valuable insights into baseline energy use and cost, laying the groundwork for subsequent analysis and recommendations.
On-Site Inspections
Complementing quantitative data collection efforts, on-site inspections were undertaken to observe the actual operation of energy systems and identify potential inefficiencies. Trained auditors conducted detailed assessments of HVAC equipment, lighting installations, and control systems, paying close attention to factors such as maintenance practices, control settings, and user behaviors. These on-site inspections provided crucial insights into discrepancies between design specifications and real-world performance, informing targeted interventions to optimize energy efficiency.
Qualitative Insights
In addition to quantitative data collection, qualitative insights were gleaned through interviews with key personnel involved in facility operations. Discussions with facility managers, maintenance staff, and frontline healthcare professionals provided invaluable perspectives on operational practices, system performance, and perceived areas of energy inefficiency. By engaging stakeholders in qualitative discussions, the audit team gained a nuanced understanding of the operational challenges and opportunities for improvement within the hospital environment.
Analysis of Conservation Measures
Energy conservation measures identified through data analysis and on-site assessments were subjected to rigorous evaluation for their cost-effectiveness and potential impact. Advanced analytical techniques were employed to calculate projected energy savings, associated costs, payback periods, and return on investment for each proposed measure. Moreover, the environmental impact of implementing these measures was assessed, with a focus on estimating the reduction in greenhouse gas emissions attributable to energy savings. This comprehensive analysis enabled the identification of strategic measures with the greatest potential for reducing energy costs and mitigating environmental impact.
Recommendations Development
Based on the findings of data analysis, on-site inspections, and stakeholder consultations, a set of prioritized recommendations was developed. Each recommendation was meticulously crafted to address specific energy inefficiencies while aligning with the hospital's operational requirements and financial constraints. An investment-grade analysis was conducted for each recommendation, providing hospital management with reliable and actionable information for decision-making. By presenting evidence-based recommendations supported by quantitative analysis and stakeholder input, the audit team facilitated informed decision-making and strategic planning for enhancing energy efficiency within the hospital.
Results
Efficient energy management strategies have been increasingly recognized as essential components of sustainable operations in various sectors, including healthcare. The ASHRAE Level 2 Energy Audit of the anonymized regional hospital provides valuable insights into the current state of the hospital's energy systems, shedding light on areas of efficiency and potential vulnerabilities. The results are organized into two primary categories: heating and cooling systems, each revealing crucial findings that inform strategic energy management decisions [8].
Heating System
The audit revealed that the hospital's heating system is robust and well-maintained, comprising three hot water boilers and two steam boilers. These boilers, installed just four years prior to the audit, were found to operate efficiently, meeting the facility's heating demands effectively. Notably, the boilers feature full redundancy, ensuring uninterrupted operation even during equipment maintenance or unexpected failures. The steam boilers, operating at 65 psi, play critical roles in sterilization processes and maintaining humidity levels in air handling units, essential for patient care and safety. Furthermore, the audit reported favourable conditions of condensate receivers and steam traps, indicating proactive maintenance practices and optimal system performance.
Cooling System
In contrast to the heating system, the audit identified significant concerns regarding the redundancy of the hospital's cooling system. The facility relies on two water-cooled chillers, two air cooled chillers, and a dedicated chiller for MRI equipment cooling. Despite regular maintenance and diligent chemical treatment of the chilled water loop, the audit highlighted the absence of redundancy within the cooling infrastructure. All cooling equipment is essential to meet peak demand, leaving no spare capacity to accommodate potential equipment failures or scheduled maintenance activities. Notably, the original design of the hospital included provisions for additional cooling capacity, such as a third water-cooled centrifugal chiller and expanded cooling tower capacity. However, these provisions were not implemented, exacerbating the lack of redundancy in the current cooling system configuration. Furthermore, facility staff expressed a preference for adding an air-cooled chiller to address the redundancy issue effectively. An air-cooled chiller would provide supplemental cooling capacity during shoulder seasons and cold weather conditions without the need to activate the cooling towers, thereby enhancing operational f lexibility and resilience. The comprehensive findings of the energy audit underscore the critical importance of strategic energy management in healthcare facilities. By elucidating the strengths and vulnerabilities of the hospital's energy systems, the audit results provide a roadmap for targeted interventions to enhance energy efficiency, operational continuity, and environmental sustainability. Furthermore, the findings serve as a catalyst for informed decision-making and resource allocation, guiding future investments in energy infrastructure and technology upgrades.
In summary, the results of the ASHRAE Level 2 Energy Audit offer actionable insights and recommendations to optimize energy utilization, reduce operational risks, and advance the hospital's commitment to sustainable practices. Through proactive energy management initiatives and stakeholder collaboration, the hospital can strengthen its resilience, improve patient care outcomes, and contribute to a greener and healthier future.
Discussion
In the process of conducting an energy audit to gain valuable insights, critical parameters for analysis encompass the building's energy consumption history, HVAC system efficiency, lighting system types and usage, efficiency of appliances and equipment, and the effectiveness of control systems in managing energy use. Additionally, examining the building envelope for insulation quality and potential thermal losses, along with assessing water heating systems and usage, contributes to overall savings. Renewable energy opportunities, occupant behavior affecting energy utilization, regular maintenance practices, and regulatory compliance with energy standards are also pivotal factors that drive energy optimization in buildings, particularly institutional infrastructures like healthcare facilities [9].
Utility data analysis stands as a cornerstone in the energy audit process, especially within healthcare facilities such as hospitals, where energy needs are complex and continuous. This analysis entails scrutinizing energy usage patterns through utility bills, pinpointing areas of unusual or peak energy consumption. It facilitates benchmarking the hospital's energy performance against similar facilities, informing cost-saving strategies by identifying peak demand periods and inefficiencies across various systems and departments. Furthermore, it establishes a baseline for evaluating the effectiveness of any implemented energy conservation measures, ensuring that the hospital can track progress and quantify the benefits of energy-saving initiatives over time [10].
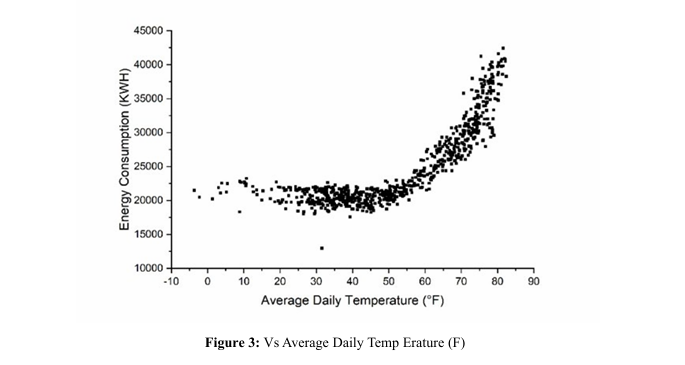
Analyzing kWh (kilowatt-hour) consumption in relation to daily average temperatures yields insights into energy usage patterns, particularly in heating and cooling systems. Typically, there exists a correlation between temperature fluctuations and energy consumption. During colder months, when temperatures drop, heating systems tend to operate more intensely to maintain comfortable indoor temperatures, resulting in increased kWh consumption. Conversely, in warmer months, higher temperatures lead to heightened usage of cooling systems, such as air conditioning, also resulting in higher kWh consumption. Conducting a kWh vs. daily average temperature analysis requires historical data on both electricity consumption (in kWh) and daily average temperatures for the area over a specific period, typically spanning multiple years. By plotting this data on a graph, trends and correlations between energy usage and temperature changes become observable.
This analysis is particularly valuable for identifying seasonal patterns in energy consumption, optimizing energy usage, and implementing strategies for energy efficiency and cost savings, such as adjusting thermostat settings, upgrading insulation, or optimizing HVAC systems. Additionally, it aids in forecasting future energy needs and planning for peak demand periods. Figure 3 demonstrates that below a temperature of 54°F, the daily kWh consumption remains constant at 21,000 kWh regardless of temperature fluctuations, indicating a baseline level of electricity consumption independent of temperature, likely representing the base load electricity usage for non-temperature-related activities. Above the threshold temperature of 54°F, the daily kWh consumption increases linearly with an increase in temperature, suggesting that temperature significantly impacts electricity consumption, particularly concerning the operation of heating or cooling systems. The moderately strong positive correlation (correlation coefficient: 0.7978) between kWh consumption and temperature underscores this relationship.
The audit results lay the groundwork for a comprehensive discussion regarding the hospital’s current energy management practices and the implications of the identified gaps. While the efficient performance of the heating system indicates successful integration of advanced technologies in a relatively new infrastructure, concerns arise regarding the cooling system’s lack of redundancy. Operational disruptions in the cooling system could have critical consequences for patient care and safety. The preference of the facility staff for an air-cooled chiller as a redundancy measure, as opposed to completing the originally planned third water-cooled centrifugal chiller and tower cell, offers a strategic direction that leans towards operational flexibility. The installation of an air cooled chiller for shoulder days can avoid the inefficiencies and maintenance complexities associated with scaling up cooling tower operations during mild weather conditions. Further discussion delves into the trade-off between energy efficiency and reliability. While the current systems demonstrate energy efficiency, their robustness during peak load conditions or equipment downtime remains vulnerable. The recommendation of an additional chiller addresses reliability concerns but also necessitates evaluation for energy efficiency during partial load conditions, which are more frequent.
Moreover, the integration of recommendations arising from energy audits into existing hospital operations must proceed with minimal service interruption. Implementing new systems or upgrades may necessitate staff training for operations and maintenance, reflecting an ongoing commitment to energy-efficient practices. Finally, the f inancial aspects of proposed improvements cannot be overlooked. The audit's recommendations are accompanied by an investment analysis; however, practical realization requires careful budgeting, possibly seeking incentives or grants aimed at enhancing healthcare facilities’ energy efficiency. The discussion extends to the environmental benefits of reduced energy consumption and greenhouse gas emissions, aligning the hospital’s operations with broader sustainability goals. In the broader context of the healthcare industry, this discussion contributes to the dialogue on how energy audits can inform not only immediate actions but also strategic planning for future expansions or renovations, underpinning the integration of energy-efficient and reliable energy systems in healthcare facilities. It underscores the importance of balancing operational effectiveness, patient comfort and safety, economic viability, and environmental responsibility in managing hospital energy systems.
Quantitative Findings
Table 1 summarizes the annual energy consumption and associated costs for electricity and natural gas usage in the specified area. The area's electricity consumption totals 8,814,894 kilowatt-hours (kWh), resulting in an annual cost of $827,667 at an average rate of $0.094 per kWh. Conversely, natural gas consumption amounts to 652,457 therms, with an annual cost of $191,725 at an average rate of $0.29 per therm. Overall, the combined energy consumption for electricity and natural gas reaches 95,308 Million British Thermal Units (MMBTU) annually, incurring a combined annual cost of $1,019,392 at an average rate of $10.70 per MMBTU.
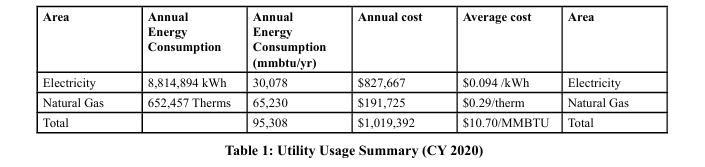
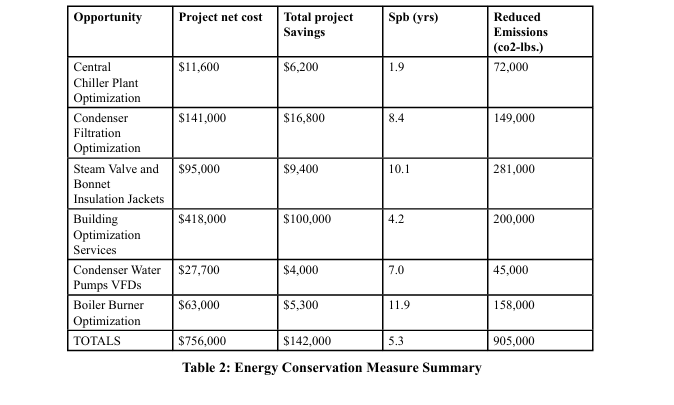
Table 2 outlines various optimization projects aimed at enhancing energy efficiency and reducing emissions within the facility. These projects include chiller plant optimization, filtration enhancement, insulation installation, and pump upgrades. Initial investments for these projects range from $11,600 to $418,000. However, they are projected to yield substantial savings and emissions reductions. The payback periods for these investments range from 1.9 to 11.9 years, with an exact average payback period calculated at 5.3 years. Collectively, these projects require a net investment of $756,000 and are expected to generate $142,000 in annual savings while reducing CO2 emissions by an estimated 905,000 pounds. This underscores a significant commitment to sustainability and efficiency, with a focus on both financial and environmental benefits.
Conclusion
The ASHRAE Level 2 Energy Audit of the regional hospital underscores a commendable commitment to energy efficiency evident in its modern heating system and integration of best practice energy-saving technologies. However, the audit reveals critical vulnerabilities, particularly in the cooling system's lack of redundancy, emphasizing the need for continuous improvement. Key findings highlight the reliability and efficiency of the hospital's available chillers in the cooling system. The recommendation to incorporate an additional air-cooled chiller is essential for enhancing operational resilience, particularly during peak demand or equipment malfunctions. heating system but raise concerns about the complete reliance on available chillers in the cooling system. The recommendation to incorporate an additional air-cooled chiller is essential for enhancing operational resilience, particularly during peak demand or equipment malfunctions.
The economic analysis underscores the importance of weighing the initial costs of proposed measures against long-term savings in energy consumption and mitigation of risks due to system downtime. Improved energy management and strategic investments The economic analysis underscores the importance of weighing the initial costs of proposed measures against long-term savings in energy consumption and mitigation of risks due to system downtime. Improved energy management and strategic investments in efficient technologies are expected to enhance the hospital's sustainability and financial stewardship. Moreover, these findings contribute to the broader discourse on sustainability in healthcare operations, emphasizing the importance of energy efficiency measures and redundancy planning for healthcare facilities. Aligning with global trends, proactive energy management practices are crucial for maintaining optimal performance, ensuring patient care services, and fulfilling environmental responsibilities in the evolving landscape of healthcare operations. In conclusion, the comprehensive audit and analysis reaffirm the necessity of a proactive and nuanced approach to energy management in hospitals. It underscores the ongoing need for careful planning, effective maintenance, and forward-thinking investments to sustain optimal performance and meet environmental responsibilities in healthcare operations [11].
References
1. Al Rashdi, S. A., Sudhir, C. V., Basha, J. S., Saleel, C. A., Soudagar, M. E. M., Yusuf, A. A., ... & Afzal, A. (2022). A case study on the electrical energy auditing and saving techniques in an educational institution (IMCO, Sohar, Oman). Case Studies in Thermal Engineering, 31, 101820.
2. Bawaneh, K., Ghazi Nezami, F., Rasheduzzaman, M., & Deken, B. (2019). Energy consumption analysis and characterization of healthcare facilities in the United States. Energies, 12(19), 3775.
3. Al-Ajlan, S. A. (2009). Energy audit and potential energy saving in an office building in Riyadh, Saudi Arabia. Journal of King Saud University-Engineering Sciences, 21(2), 65-74.
4. Teke, A., & Timur, O. (2014). Assessing the energy efficiency improvement potentials of HVAC systems considering economic and environmental aspects at the hospitals. Renewable and Sustainable Energy Reviews, 33, 224-235.
5. Liu, A., Miller, W., Crompton, G., & Ma, Y. (2020, November). Principles to define energy key performance indicators for the healthcare sector. In 2020 International Conference on Smart Grids and Energy Systems (SGES) (pp. 898-903). IEEE.
6. Sahamir, S. R., Zakaria, R., faizal Omar, M., Shakri, M. R., Chughtai, M. W., Mustafar, M., & Rooshdi, R. R. R. M. (2019, September). Energy efficiency criteria for planning and design of green hospital buildings rating system. In IOP Conference Series: Materials Science and Engineering (Vol. 620, No. 1, p. 012082). IOP Publishing.
7. Darshan, A., Girdhar, N., Bhojwani, R., Rastogi, K., Angalaeswari, S., Natrayan, L., & Paramasivam, P. (2022). Energy audit of a residential building to reduce energy cost and carbon footprint for sustainable development with renewable energy sources. Advances in civil engineering, 2022(1), 4400874.
8. Abdallah, A. S. H., Makram, A., & Nayel, M. A. A. (2021). Energy audit and evaluation of indoor environment condition inside Assiut International Airport terminal building, Egypt. Ain Shams Engineering Journal, 12(3), 3241-3253.
9. Ali, S. B. M., Hasanuzzaman, M., Rahim, N. A., Mamun, M. A. A., & Obaidellah, U. H. (2021). Analysis of energy consumption and potential energy savings of an institutional building in Malaysia. Alexandria Engineering Journal, 60(1), 805-820.
10. Alajmi, A. (2012). Energy audit of an educational building in a hot summer climate. Energy and buildings, 47, 122-130.
11. Sahamir, S. R., Zakaria, R., faizal Omar, M., Shakri, M. R., Chughtai, M. W., Mustafar, M., & Rooshdi, R. R. R. M. (2019, September). Energy efficiency criteria for planning and design of green hospital buildings rating system. In IOP Conference Series: Materials Science and Engineering (Vol. 620, No. 1, p. 012082). IOP Publishing.