Case Study - (2024) Volume 9, Issue 5
Effectiveness of Cognitive Behavioral Therapy (CBT) Combined with Brief Hypnotherapy (BH) in the Treatment of Persistent Enuresis in Adolescence in an Institutional Setting, Literature Review and Case Study
2Centre for Psychotraumatology and Mediation (CPM), affiliated with SIPM: Swiss Institute of Postgrad, Switzerland
3Centre for Psychotraumatology and Mediation (CPM), Ottawa, ON,, Canada
4Centre for Psychotraumatology and Mediation (CPM), Yaounde, Cameroon,, filiale de l’IPM-International, Switzerland, Italy
5Children Hospital of Eastern Ontario (CHEO), Ottawa, ON, Canada., Canada
Received Date: Apr 24, 2024 / Accepted Date: May 01, 2024 / Published Date: May 14, 2024
Abstract
Primary enuresis, commonly known as “bedwetting”, is a common disorder affecting around 15-20% of children aged 5 years [1]. It is defined as the repeated occurrence, at least twice a week for at least 3 consecutive months of episodes of involuntary urination into the bed or clothes during sleep, in a child aged over 5 [2,3].
Introduction
Primary enuresis, commonly known as “bedwetting”, is a common disorder affecting around 15-20% of children aged 5 years [1]. It is defined as the repeated occurrence, at least twice a week for at least 3 consecutive months of episodes of involuntary urination into the bed or clothes during sleep, in a child aged over 5 [2,3]. These repeated nocturnal episodes are a source of psychological distress and functional repercussions for the child in social, emotional, and sometimes academic terms. In addition to the discomfort and fatigue caused, enuresis can lead to feelings of shame, lowered self-esteem, and social isolation, with an impact on friendships and academic success [4,5]. Although in most cases of enuresis regresses spontaneously before the age of 10 as the bladder and nervous system mature, it can persist into adolescence and even adulthood [5]. In adolescents, this disorder is a source of great distress and altered psycho-social functioning. Enuresis then becomes highly disabling at a crucial time in the development of identity and relationships [4]. Primary enuresis is therefore a common disorder that can be very disabling if it persists beyond childhood, which is why it is so important to offer appropriate, personalized treatment to older children and adolescents with enuresis.
A male predominance is consistently observed, with a sex ratio of approximately 2:1 in favour of boys [6]. The risk factors associated with the persistence of primary enuresis in adolescence combine genetic, medical, and psychosocial factors [6]. Genetically, there is often a family history of enuresis. In medical terms, certain pathologies such as urinary tract infections or chronic constipation are contributing factors. Finally, at a psychosocial level, psychological disorders such as anxiety or depression, as well as family stress, are correlated with the chronicization of this disorder [6]. Thus, the persistence of primary enuresis in adolescence is rooted in multiple factors, justifying comprehensive medical and psychological treatment tailored to this age group.
Various drug treatments for primary enuresis have been studied, including desmopressin, imipramine, and oxybutynin [7]. Desmopressin is an antidiuretic hormone analogue that reduces urine production at night. Tricyclic antidepressants such as imipramine increase the wake-up threshold. Anticholinergics such as oxybutynin reduce bladder hyperactivity. While these drugs have demonstrated some short-term efficacy, studies have highlighted their significant side-effects, digestive problems, headaches, and dizziness [7]. What is more, their long-term efficacy is questionable, since in most cases the effect wears off when treatment is stopped. Given these limitations, nondrug approaches have been explored in recent years, notably cognitive behavioral therapy (CBT) and hypnosis [8,9]. CBT works on thoughts and behaviors to modify negative self-image, anxiety and poor bladder and bowel habits. Hypnosis acts at an unconscious level by increasing the child’s motivation and sphincter control at night. Studies suggest promising results for these methods, with lasting positive effects and no side effects [8,9]. They therefore appear to be relevant therapeutic alternatives to be explored further, particularly in adolescents with primary enuresis.
Although CBT and hypnosis have shown encouraging preliminary results in the treatment of primary enuresis, few studies to date have looked specifically at their effectiveness in adolescents with chronic enuresis [8,9]. Persistent enuresis in adolescence, which is resistant to previous treatments, poses a real therapeutic problem, and its psychosocial repercussions at this age make it a major clinical issue. In view of this, it seems appropriate to evaluate more precisely the value of CBT and hypnosis in the management of enuresis in older children and adolescents.
Our case study aims to shed light on this issue through the presentation of a 15-year-old girl suffering from chronic primary enuresis, resistant to previous drug treatments. We will detail the treatment methodology, combining CBT and hypnosis, implemented over a three-month period. The results obtained will be presented. Finally, the discussion will analyze these results in the light of current data in the literature to assess the value of this therapeutic approach and to consider the prospects for future controlled studies in this population.
Case Study of This Study
The case study focuses on a 15-year-old girl, whom we will refer to as “Ngonda” for the sake of anonymity and confidentiality. She was admitted to the Pedagogical and Therapeutic Center of Dombresson (CPTD), Borel Foundation, to receive appropriate care from a multidisciplinary team in an institutional setting. This care was provided under the guidance of the therapeutic team of the Department of Child and Adolescent Psychiatry of the Neuchâtel Psychiatric Center (CNPea), in collaboration with the educational team of CPTD.
Ngonda was admitted due to two main issues. Firstly, she suffers from primary enuresis, meaning she involuntarily wets the bed despite her age. Secondly, she experiences significant academic difficulties. Ngonda’s parents have been divorced since she was 12, following notable marital conflicts, followed by a one year separation. The child psychiatry team from CNPea joined Ngonda’s care one year after her admission to CPTD. She had been placed at CPTD due to psychosocial distress related to family issues, mental health disorders, behavioral disorders, learning difficulties, and academic failures.
Psychiatrically, Ngonda has been known to the outpatient services of CNPea since her primary school years due to extreme shyness classified as social phobia since the age of 10 (4th and 5th grades). She also exhibits symptoms of depression, difficulties in academic learning, and persistent primary enuresis despite various previous outpatient treatments, including pharmacological and psychodynamic and family-inspired psychotherapy.
Ngonda’s family psychiatric history reveals that her mother has also been treated for anxiety disorders and underwent psychiatric treatment and psychodynamic psychotherapy. Ngonda’s mother also experienced primary enuresis in her childhood but attributed her recovery and control to maturity rather than specific therapy. Her enuresis completely stopped at the age of 12, after her first menstruation. However, she is concerned that Ngonda continues to have enuresis issues at the age of 15, despite also experiencing her first menstruation at 12, like her mother.
In addition to persistent and treatment-resistant enuresis, Ngonda’s mother observes that her daughter is becoming increasingly anxious, avoidant, and significantly lacks selfesteem in the presence of peers and adults. This situation negatively impacts her academic performance, and her mother fears that Ngonda might drop out of school due to her repeated absences caused by avoidance behavior. Ngonda also presents symptoms of depression, including dark thoughts. To address these issues, her mother requested the admission of her daughter to the Borel Foundation, at CPTD, where she can receive integrated psychiatric and psychotherapeutic care (PPTI) as well as specialized education from a highly qualified team.
Objectives and Methodology
3.1 Objectives
3.1.1 Main Objective: Demonstrate the effectiveness of Cognitive-Behavioral Therapy (CBT) combined with Brief Hypnotherapy (BH) in managing persistent primary enuresis in this adolescent
3.1.2 Secondary Objectives
Show that defining a clear therapeutic framework improves treatment adherence and compliance.
Highlight the importance of positive reinforcement to facilitate the transition to cleanliness.
Demonstrate the impact of this intervention on social anxiety, self-esteem, secondary depression, and associated learning disorders
3.2 Method
3.2.1 Study Type
This is an interventional case study aimed at evaluating the effectiveness of a treatment involving Cognitive-Behavioral Therapy (CBT) combined with Brief Hypnotherapy (BH) for a 15-year-old adolescent with resistant primary enuresis.
3.2.2 Procedure for Initiating Placement in an Institutional Setting
After a two-week observation period at CPTB, a comprehensive intervention for Ngonda was decided during a collaborative synthesis involving the therapeutic, educational, and school teams, under the authority appointed by the judge of the cantonal court of Neuchâtel. In Switzerland, placing a child in a therapeutic care institution due to behavioral problems and learning difficulties is regulated by Article 426, paragraph 1 of the Swiss Civil Code (CC) [10]. This article allows the placement of a person in an appropriate institution when assistance or necessary treatment cannot be provided otherwise due to psychological disorders, mental impairment, or severe neglect. The decision for such placement is usually made by the child and adult protection authority, often the magistrate judge in many cantons. This provision is part of the legal framework for child and adult protection in Switzerland.
3.2.3 Plan Using Cognitive-Behavioral Approach (CBT) and Brief Hypnotherapy (BH)
The treatment, focusing on CBT and BH, is divided into four phases for Ngonda
3.2.4 Establishment of a Good Alliance and Personalized Therapeutic Framework
After a year at CTPD, Ngonda experienced a relational and educational environment adapted to her condition by welltrained and experienced educators. This framework established a good interpersonal and therapeutic relationship to build Ngonda’s trust, addressing the sensitive issue of enuresis at the age of 15. Despite the ongoing presence of this embarrassing issue, Ngonda felt relatively more comfortable at CTPD than at the public school in the community.
Following a case review between the CTPD team and the Child Psychiatry team of the Department of Child Psychiatry at CNPea, a therapeutic reframe was established. Three sessions were then dedicated to building trust, pediatric psychiatric evaluation, and psychoeducation by the Child Psychiatry team responsible for Ngonda’s Integrated Psychiatric and Psychotherapeutic Treatment (IPPT) using CBT and BH. After these three sessions, the focus shifted to more action and techniques in CBT and BH, incorporating exercises during and outside the sessions as homework. The therapeutic processes in terms of CBT and BH unfolded in four phases: the learning phase, stabilization of morbid symptoms, consolidation of the desired state, and generalization of learning to other areas of the adolescent’s life.
3.2.5 Learning Phase of Hypnosis and Self-Hypnosis
In this phase, Ngonda learned how her cognitive and emotional processes functioned. Her thoughts and beliefs about enuresis shaped how she perceived herself, affecting her emotions and behaviors of shyness, avoidance, and shame at school. The connection between CBT and BH was explained and applied to Ngonda’s experiences with enuresis. Instead of explicitly mentioning hypnosis, the team utilized a technique referred to as “hypnosis without hypnosis” for this 15-year-old adolescent.
The learning process involved understanding cognitive and emotional functioning and applying these concepts to Ngonda’s experiences with enuresis. The link between CBT and BH was established without delving too deeply into explanations, considering the potential anxiety associated with discussing hypnosis with an adolescent experiencing enuresis during sleep.
The initiation to hypnosis was discussed under parental consent for minors like Ngonda. Depending on individual hypnotizability, the learning process could vary in duration. After initial sessions of inducing light hypnotic trances, Ngonda was guided to master the sessions. Homework assignments included exercises under self-hypnosis without explicitly mentioning the term “hypnosis,” aligning with the Milton Erickson approach.
3.2.6 Stabilization Phases
Once the desired behavior was achieved after several sessions of brief hypnotherapy, the team ensured that Ngonda had control over the desired state-being free of enuresis. This control had to be verifiable, measurable, and reproducible over a period of 3 to 4 weeks without relapse into undesirable morbid behavior. Only after achieving stability could the intervention move on to the consolidation phase.
3.2.6 Consolidation Phase
The consolidation phase involved ensuring the stability of the desired behavior in the institutional setting for a minimum of 21 days or 3 weeks. Ngonda needed to demonstrate no enuresis for at least 21 consecutive days. This absence of enuresis needed to be verifiable and measurable by Ngonda, her close ones, the educational and pedagogical team, and the psychiatrist in charge of CBT and BH at the Borel Foundation. If this phase maintained without relapse for 21 to 30 days, the intervention progressed to the generalization phase of the desired behavior to other spheres in the emotional, educational, and social realms, referred to as the generalization of acquired skills.
3.2.7 Phase of Generalization of Acquired Skills
In the specific case of a 15-year-old adolescent placed in the therapeutic and educational center of Dombresson (CTPD), the generalization of the desired behavior on the academic level is one of the main objectives. This occurs after reaching the level of recovery of behaviors or the desired state as desired by the patient, her family, and the institution. The generalization of desired behaviors goes beyond the scope of the primary diagnosis to positively impact secondary psychiatric diagnoses, as mentioned in the anamnestic summary of our case study, namely social anxiety disorder (SAD), generalized anxiety disorder (GAD), and depressive disorder (DD).
This phase of generalization of behaviors, cognitions, and positive emotions was facilitated using several affective bridges (11). The utilization of affective bridges through positive emotions and associated mental images was carried out by the patient in a state of fractionated, light, and deep hypnotic trance. This involved a dynamic interplay, incorporating techniques from CBT such as relaxation, cognitive restructuring, identification, and desensitization of negative emotions related to the morbid state, and reprocessing or reprogramming of information in the form of beliefs, thoughts, or self-images. Information from BH, such as induction of fractionated, light, or deep hypnotic trance states, accompanied by suggestions involving visualizations and affective and emotional bridges, was integrated. All these techniques, combining CBT and BH, were implemented during sessions in an atmosphere of strong therapeutic alliance. The approach appeared both playful and therapeutic, using word associations, colors, and pleasant sensations.
Through this flow of mental images, positive thoughts, and induced positive emotions, we assisted this adolescent in transitioning from unpleasant states of consciousness associated with the shame of enuresis to pleasant states of consciousness linked to waking up clean without urine in her bed or on her pajamas. By helping her associate the physical and psychological shame of being wet with urine with phobic and avoidance behaviors in certain situations and her joy in a positive emotional state without urine in her bed and body, we aided her in imagining scenarios during sessions.
Thanks to these exercises conducted during sessions and as homework, she achieved a drastic reduction in her anxiety and depressive disorders, and an improvement in her self-esteem over 3 to 4 sessions, with one session per week. Observational clinical data on her condition were self-evaluated on sheets by Ngonda herself under the supervision of her reference educator. Hero-evaluation was conducted by the child psychiatrist during the CBT and BH sessions.
3.3 Materials for Data Collection
-Tape recorder, audio cassettes, and well-organized note-taking files.
-Various forms and sheets for data collection after the exercise, mainly used by the young patient to complete homework in the form of Relaxation and Mental Imagery (RMI) Exercises, which are essentially Hypnorelaxation Exercises (HE) practiced again at home by Ngonda. She learned to do this with great ease during her sessions with me in the learning phase mentioned above.
In these sheets, she gives herself a score of “1” when, after the hypnorelaxation exercise, she spends a night without enuresis, waking up clean. She gives herself a score of “0” when she wakes up to find that she wet the bed and her pajamas are soaked. When presenting this score to her reference educator, she accumulates points for future rewards for her efforts and progress in staying dry without wetting the bed.
Psychometric assessment for comorbid disorders related to her enuresis: GAD, DD, and SAD, using the following questionnaires and scales: Hamilton Anxiety Scale (HAS), Beck Depression Inventory (BDI), and Liebowitz Social Anxiety Scale (LSAS). She also brings the results of her cleaning and arranging efforts in the shared room and her bed to each session to demonstrate the level of her therapeutic progress to the child and adolescent psychiatrist, who takes the opportunity to provide positive reinforcement.
Data Analysis
4. Data Analysis
- We analyzed the number of enuresis episodes per week.
- We conducted a before/after intervention comparison using appropriate statistical tests.
- We performed a time-based analysis (linear regression).
4.1 Primary Outcome Criterion
- Number of enuresis episodes per week in the institutional setting or at home with her mother during the weekend.
- The results of the case study are presented in the form of a structured report.
Results
In the treatment of persistent enuresis in the adolescent Ngonda, two contexts were compared: when she is at the Center for Pedagogy and Therapy in Dombresson (CPTD) and when she is with her mother during weekends or holidays. When Ngonda is at CPTD, she experienced enuresis crises 25 times during her sleep and successfully went through the night without enuresis 156 times, indicating a significant improvement in her urinary control through cognitive-behavioral therapy (CBT) combined with hypnosis in the institutional setting.
Similarly, during weekends and days off with her family and her mother, Ngonda showed similar results, urinating 31 times during sleep in her bed and remaining clean without wetting her bed 156 times during her family breaks with her mother. These numbers suggest that this therapeutic approach had a positive impact on managing her persistent enuresis, providing this young patient with behavioral and cognitive potential for continuous improvement in urinary control from adolescence to adulthood.
Significance of CBT and Hypnosis for the Treatment of Enuresis in Children and Adolescents
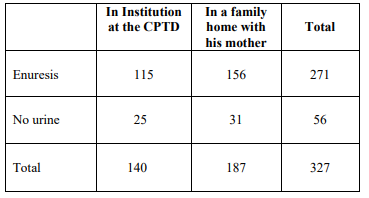
Table 1: For P-values for the presence of enuresis and absence of enuresis.
The data present a contingency table with the numbers observed for the presence/absence of enuresis in children seen at a CPTD (children’s medical-psychological center) or at their mother’s home. We tested the independence between the place (CPTD/ mother) and the presence of enuresis.
The expected values under the hypothesis of independence were calculated. The observed numbers are close to the expected numbers. The Chi2 test of independence was performed. The p-value was 0.761191. At the 5% threshold, the null hypothesis H0 of independence between location and the presence of enuresis cannot be rejected.
In conclusion, this analysis shows no significant difference between the proportion of enuretic children seen in CPTD or at their mother’s home. The data are compatible with the hypothesis of independence between these two variables. There is no statistical evidence of an effect of location on the presence of enuresis.
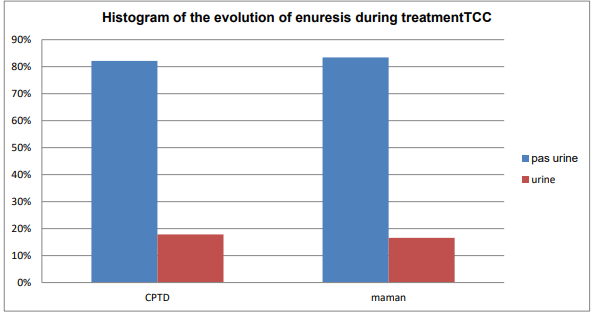
Figure I: Histogram of the evolution of enuresis during treatment.
The percentage of enuretic children was very similar in the two settings: 18% in the CPTD and 17% in the mother’s home. This could suggest that the context of the consultation (medical facility versus home) does not have a major impact on the detection of this disorder in this study. Another interpretation is that the prevalence of enuresis is relatively stable in children, whether they are seen in a CPTD or by their mother. The fact of consulting in one or the other place does not seem to significantly vary the probability of detecting this problem.
It could also be said that the place of consultation (CPTD or mother) does not constitute a risk or protective factor for enuresis in this study.
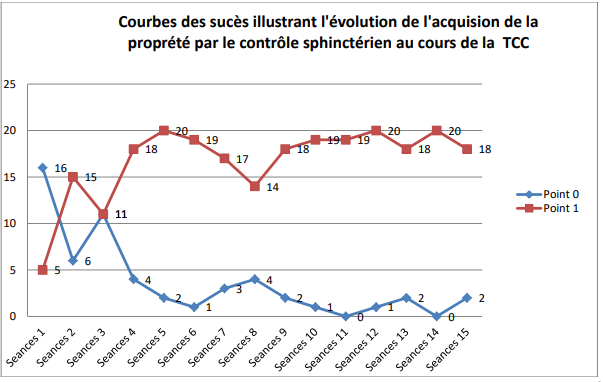
Figure 2: Course of enuresis during treatment.
6. Evolution of Enuresis and Interpretation
The evolution of enuresis during treatment can be interpreted from the provided data, which shows the frequency of urination and urine retention in the adolescent Ngonda in two different contexts: at the Center for Pedagogy and Therapy in Dombresson (CPTD) and in the presence of her mother.
The trendline suggests that, thanks to cognitive-behavioral therapy (CBT) combined with hypnosis in the institutional setting, Ngonda has gradually improved her urinary control over time. Initially, she had significant enuresis episodes, as evidenced by the high urination numbers at CPTD. However, over the course of treatment, there is a downward trend in her enuresis episodes, indicating better voluntary and involuntary control of her urination.The stabilization of urine retention numbers suggests that Ngonda has learned to successfully withhold her urine while in a state of sleep, which is a positive aspect in managing enuresis. These results demonstrate the effectiveness of CBT and hypnosis in treating persistent enuresis in this adolescent, offering an encouraging outlook for the continuous improvement of her urinary control as she continues with the treatment. However, longer-term observation in the form of follow-up would be necessary to assess the stability of these progressions and their long-term maintenance.
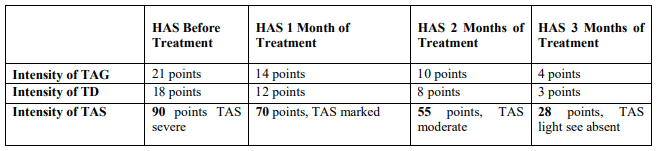
Table 2: For Results of GAD, DD, and SAD.
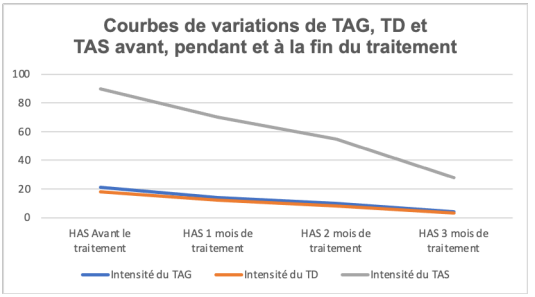
Figure 3: Variation curves for TAG, TD and TAS before, during and at the end of treatment.
Over the course of her comprehensive care, which included enuresis treatment and psychosocial interventions, there was a marked improvement in all these disorders: - SAD, which was very high at the outset, gradually decreased significantly.
- GAD and TD also regressed significantly during follow-up
This all-round positive development suggests that effective enuresis management substantially reduced the anxiety, worry and depression associated with this urinary disorder. In conclusion, this case illustrates the benefits of a comprehensive therapeutic approach, targeting both enuresis and its psychological repercussions. Treatment of the primary disorder appears to have a positive knock-on effect on the associated secondary disorders.
Discussion
According to the results of this case study, it is essential to discuss different treatment approaches for enuresis, comparing them to existing literature references. Firstly, regarding pharmacological treatment for enuresis, this case study did not introduce medication as an associated pharmacological treatment for two reasons. The first reason is the mother’s refusal, as reported in the hetero-anamnesis, citing resistance to pharmacological and mechanical treatments by the pediatrician, child psychiatrist, and psychodynamic psychotherapy. The second reason is the therapeutic, educational, and pedagogical team’s (TEPM) avoidance of medication use in cases where psychiatric disorders pose no risk of behavioral issues, such as auto or hetero-aggression, in residents with disruptive behaviors like attention deficit hyperactivity disorder (ADHD) or bipolar disorders among children and adolescents residing in the institution.
The results strongly confirm the effectiveness of cognitivebehavioral therapy (CBT) combined with hypnosis (HB). It is noteworthy that CBT and HB have shown promising results,encouraging consideration of this approach before opting for pharmacological treatments, particularly due to potential side effects associated with various medications.
As for CBT and HB for enuresis, this case study suggests that this approach can be effective in improving anal and vesical sphincter control in adolescents. This aligns with existing literature results, indicating that CBT combined with HB can be an effective strategy for enuresis management [12]. This case study also reveals the beneficial impact of hypnosis in treating enuresis in adolescents. Although less commonly used, this approach seems to offer significant advantages by reinforcing urinary control in the adolescent.
Regarding mechanical treatment for enuresis, such as alarms and low-voltage electric shocks [13]. It is important to note that in Ngonda’s case, prior management with mechanical and pharmacological treatments had not been conclusive, as reported by her mother.
Catamnesis
In terms of the follow-up after recovery from enuresis (catamnesis), we reached out to the Management and Archives department of the Therapeutic and Pedagogical Center of Dombresson (CTPD) at the Borel Foundation after 6 years. They confirmed that since the completion of the mentioned treatment by our team, the patient, Ngonda, has not experienced any relapses until her departure. The Director of the institution confirmed that after Ngonda’s three months of care by the child psychiatry team for her enuresis, she left without any recurrence of sphincter issues or anxio-depressive symptoms until the end of the current school year. He mentioned that, additionally, the adolescent successfully completed the school year at the CPTD with good results. Subsequently, she returned to her family under the care of her mother, who was responsible for her guardianship after her parents’ divorce. Ngonda also smoothly reintegrated into the community, attending a public secondary school as a day student.
As part of the Borel Foundation’s best practices, the institution’s management for children and adolescents facing psychosocial distress and academic challenges always seeks feedback on the progress of its residents from their families whenever possible.
In Ngonda’s specific case, her return to the family and reintegration into an external public secondary school occurred without difficulty. Upon completing compulsory education, she pursued vocational training, culminating in the attainment of a Federal Certificate of Competence (CFC). At the age of 21, she commenced employment immediately after successfully completing pre-employment internships, showcasing both theoretical and practical competence, in various companies within the Canton of Neuchâtel.
Conclusions
Effective Approach:
Our case study has demonstrated that CBT combined with hypnotherapy (HB) is an effective approach to improving bladder sphincter control in a 15-year-old adolescent suffering from persistent enuresis resistant to other therapeutic approaches. This approach proved particularly useful in rapidly reducing and stopping enuresis episodes without relapse. In comparison to the literature, which mentions other methods focused on CBT and pharmacological treatments, our approach appears to stand out in terms of efficacy for this specific case [14].
Holistic Approach:
Hypnocomportemental and Cognitive Therapy (THCC) combines elements of cognitive and behavioral therapy with hypnosis, offering a holistic approach that addresses both the mental and behavioral aspects of the disorder. This can be beneficial in treating the underlying causes (at the unconscious level) of enuresis and factors related to the social and familial environment of patients.
Side Effect-Free Approach:
Unlike some mechanical and pharmacological treatments, THCC carries no potential risks of medication-related side effects, making it a safer, cost-effective, and eco-friendly option.
Focus on Self-Control Learning:
Hypnosis associated with THCC can help patients develop self-control skills and selfesteem, which can be transferred to other aspects of life in adolescents.
Personalized Approach: THCC can be tailored to meet the specific needs of each patient based on their resources and history, making it a flexible and even transcultural approach, considering patients’ affiliations.
Transdiagnostic Approach:
In this study, there was no need to introduce pharmacotherapy for the treatment of secondary psychiatric disorders in this case of treatment-resistant and persistent enuresis in adolescence. This THCC approach focused on the primary diagnosis (enuresis), bringing about a rapid recovery for the adolescent, allowed her to generalize the acquired skills toward overall recovery, directly and indirectly impacting her Generalized Anxiety Disorder (GAD), Social Anxiety Scale (SAS), and Depressive Symptoms (DS) without the need for additional care in the outpatient unit for anxiety and mood disorders in children and adolescents (CNPea).
According to the literature, Social Anxiety Scale (SAS) or Social Phobia is classified by intensity in the following intervals: Moderate SAS: 56-65; Marked SAS: 66-80; Severe SAS: 81-95; Very Severe SAS: a score of 95 on the Liebowitz Social Anxiety Scale (LSAS), indicating severe social anxiety according to normative data [15]. LSAS considers a score below 56 as mild social anxiety, and a score below 28 reflects a lack of functional impact. Following treatment, Ngonda shows a significant reduction in anxious symptoms to a sub-clinical level. Clinically and compared to literature data, we can affirm that Ngonda also experienced recovery from her comorbid anxio-depressive disorders related to her enuresis [16]. The remission of enuresis was accompanied by a significant improvement in her associated anxious and depressive symptomatology. This observation aligns with the frequent comorbidity between enuresis and emotional disorders in adolescents [17].
It should be noted, however, that CBT is effective in treating depression and anxiety in adolescents [18], and hypnotherapy is also effective according to some studies [19]. We can deduce that the combination of CBT and hypnotherapy had a synergistic effect that impacted the overall mental health recovery of this adolescent who had lost hope of pursuing her education and professional development normally due to persistent enuresis resistant to outpatient treatments in child psychiatry and pediatrics.
Thanks to this THCC intervention in an institutional setting, we assisted this adolescent in overcoming her previous academic failure and the risk of harmful school dropout during the transition age, thanks to the rapid restoration of her sphincteric cleanliness and its positive repercussion on other mental health disorders comorbid to her enuresis.
In summary, our THCC approach used in this case study seems to present distinctive and remarkable advantages for the treatment of enuresis in this adolescent compared to other more conventional approaches mentioned in the literature. It offers a comprehensive approach without side effects compared to pharmacological approaches [20]. In their study on the treatment of encopresis, Biyong I and Irène Coretta Ngo Beguel [21,22] demonstrated the effectiveness of hypnocomportemental and cognitive therapy (THCC) in sphincter control in adolescents suffering from encopresis on megacolon in an institutional setting. This approach adapts to and aligns with individuals based on the unique characteristics of each patient and the medical-psychosocial, emotional, and family context. THCC promotes the learning of self-control, introspection, boosts self-esteem in the face of a disorder causing shame and peer rejection in adolescents, while allowing customization to meet the unique needs of each patient. However, it is essential to continue accumulating clinical data to confirm these benefits and better understand how THCC can be integrated into institutional and even outpatient care for treatment-resistant and persistent enuresis in adolescence.
In conclusion, this case study suggests that CBT combined with hypnotherapy can be an effective alternative approach for the treatment of persistent and treatment-resistant enuresis in adolescents. However, further controlled studies are needed to confirm these results and better understand how these approaches compare to pharmacological and mechanical treatments, considering the existing scientific literature in this field.
References
1.Butler, R. J., & Heron, J. (2008). The prevalence of infrequent bedwetting and nocturnal enuresis in childhood. A large British cohort. Scandinavian Journal of Urology and Nephrology, 42(3), 257-264.
2. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
3. Nevéus, T., von Gontard, A., Hoebeke, P., Hjälmås, K., Bauer, S., Bower, W., ... & Yeung, C. K. (2006). The standardization of terminology of lower urinary tract function in children and adolescents: report from the Standardisation Committee of the International Children’s Continence Society. The Journal of Urology, 176(1), 314- 324.
4. Joinson, C., Heron, J., & von Gontard, A. (2006). Psychological problems in children with daytime wetting. Pediatrics, 118(6), 1985-1993.
5. von Gontard, A., Equit, M., & Combs, S. (2011). Cognitive and emotional factors in children with nocturnal enuresis: a review. Acta Paediatrica, 100(3), 368-377.
6. Yeung, C. K., Sreedhar, B., Sihoe, J. D., & Sit, F. K. (2004). Characteristics of primary nocturnal enuresis in adults: an epidemiological study. BJU International, 93(3), 341-345.
7. Caldwell, P. H., Nankivell, G., & Sureshkumar, P. (2013). Simple behavioural interventions for nocturnal enuresis in children. Cochrane Database of Systematic Reviews, 7, CD003637.
8. Glazener, C. M., Evans, J. H., & Peto, R. E. (2005). Complex behavioural and educational interventions for nocturnal enuresis in children. Cochrane Database of Systematic Reviews, 2, CD004668.
9. Konstantinou, K., & Johnson, M. I. (2009). The role of cognitive–behavioral therapy in the management of nocturnal enuresis: a systematic review and meta-analysis. Neurourology and Urodynamics, 28(5), 395-401.
10. Code civil suisse (CC) , Article : 426, alinéa 1, Révisé et est entré en vigueur le 1er janvier 2020.
11. Spiegel, D., & Spiegel, H. (2004). Trance and treatment: Clinical uses of hypnosis (2nd ed.). American Psychiatric Publishing. - Ce livre est écrit par deux experts en hypnose et offre des perspectives cliniques sur l’utilisation de l’hypnose dans le traitement.
12. American Academy of Child and Adolescent Psychiatry (AACAP). (2013). Practice parameter for the assessment and treatment of children and adolescents with enuresis. Journal of the American Academy of Child and Adolescent Psychiatry, 52(8), 903–909.
13. Leebeek-Groenewegen, A., Blom, J., Sukhai, R., & Hirasing, R. (2020). Efficacy of bladder training with and without dry bed training for nocturnal enuresis in children: Randomized controlled trial. Journal of Pediatric Urology, 16(6), 715-722.
14. Banerjee, S., Srivastav, A., & Palan, B. (1993). Hypnosis and self-hypnosis in the management of nocturnal enuresis: a comparative study with imipramine therapy. American Journal of Clinical Hypnosis, 36(2), 113-119.
15. Kiddoo, D., Sawyer, J., Friesen, C., & Klassen, T. P. (2021). Combined enuresis alarm and desmopressin versus enuresis alarm monotherapy for nocturnal enuresis in children. Cochrane Database of Systematic Reviews, 2021
16. Olivares, J., Sánchez-García, R., & López-Pina, J. A. (2009). The Liebowitz Social Anxiety Scale for Children and Adolescents. Psicothema, 21(3), 486–491.
17. Banerjee, S., Srivastav, A., & Palan, B. (1993). Hypnosis and self-hypnosis in the management of nocturnal enuresis: a comparative study with imipramine therapy. American Journal of Clinical Hypnosis, 36(2), 113-119.
18. Joinson, C., Heron, J., Emond, A., & Butler, R. (2007). Psychological problems in children with bedwetting and combined (day and night) wetting: A UK population-based study. Journal of pediatric psychology, 32(5), 605-616.
19. Weisz, J. R., McCarty, C. A., & Valeri, S. M. (2006). Effects of psychotherapy for depression in children and adolescents: a meta-analysis. Psychological bulletin, 132(1), 132–149.
20. Houts, A. C., Berman, J. S., & Abramowitz, H. (1994). Effectiveness of psychological and pharmacological treatments for nocturnal enuresis. Journal of consulting and Clinical Psychology, 62(4), 737–745
21. Bollard, J. & Nettelbeck, T. (1988). A component analysis of dry-bed training for treatment for bedwetting. Behaviour Research and Therapy, 26(4), 383-390.
22. Issack Biyong, Irène Coretta Ngo Beguel B., Michel Botbol (2023). Brief Hypnosis Therapy of Encopresis on megacolon in a Psychiatric Institution for Children and Adolescents. Medcina Intern 5, 182.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



