Case Report - (2023) Volume 8, Issue 11
Bulbar Stenosis Revealing Duodenal Ulcer Disease In A Child: About A Case
2Department of Radiology, Faculty of Medicine of Tlemcen, University of Tlemcen Aboubakr Belkaid, CHU Tidjani Damerdji, Tlemcen, Algeria
3Department of Child Surgery, Faculty of Medicine of Tlemcen, University of Tlemcen Abou Bekr Belkaid, EHS Mother Child, Tlemcen, Algeria
Received Date: Nov 11, 2023 / Accepted Date: Nov 14, 2023 / Published Date: Nov 24, 2023
Abstract
Duodenal ulcer disease is relatively rare in children. Can be discovered at the stage of bulbar stenosis which is a complication whose treatment is essentially surgical; it is particularly mentioned in the case of chronic vomiting. A young child of 11 years old was admitted to the hospital 08 years ago for chronic vomiting associated with weight loss. He had a personal history of failure to thrive at the age of 6 without obvious etiology, and occasional consumption of shisha. The normal clinical examination contrasted with a biological inflammatory syndrome. An esogastroduodenal endoscopy carried out showed a tight pyloro-bulbar stenosis that could not be overcome, the biopsies taken showed non-specific duodenitis and absence of signs of malignancy, justifying sequential treatment with additional exploration: abdominal-pelvic scan and an esogastroduodenal transit confirming the stenosis. fibrous. Surgical treatment was carried out by a Mikulicz pyloroplasty, with good postoperative outcomes. The child remained asymptomatic. At the age of 20, occurrence of another complication of his ulcer disease such as heavy digestive bleeding requiring hospitalization in the gastroenterology department. The evolution was favorable under massive transfusion and treatment including amoxicillin, clarithromycin and metronidazole (14 days) and omeprazole (7 weeks). An endoscopic check one month later showed complete healing of the ulcer.
Keywords
Bulbar stenosis, Digestive endoscopy, Gastrointestinal bleeding, Ulcer
Introduction
Gastroduodenal ulcer disease (UGD) in children is less common than in adults; few data are published in terms of its prevalence, its clinical manifestations, risk factors and its treatment. We distinguish between primary UGD and secondary UGD, encountered during treatments with gastrotoxic drugs or in cases of stress [1]. Primary peptic ulcers in children is observed in children with an average age of around eleven years and are more often located in the duodenal bulb. The main causes of peptic ulcer in children are Helicobacter Pylori infection which occurs in childhood through transmission, most often within the family, the use of anti-inflammatories and the consumption of tobacco and alcohol.
The diagnosis is essentially endoscopic. Complications are dominated by digestive hemorrhages, perforation and pylorobulbar stenosis which make the disease serious. The aim of this work was to draw attention to this revealing mode of pediatric duodenal ulcer disease.
Patient and Observation
2.1. Patient information
The child M H, aged 13, male, with a medical history of failure to thrive at the age of 6 years, explored at the time in the pediatric department without any obvious etiology, was found in this case to be celiac disease, ruled out by the negativity of the results of the Oesogatroduodenal fibroscopy with duodenal biopsies and the immunological assessment of anti-transglutaminases AC. On the family level, father and mother do not present any clinically obvious pathology. Consulted the emergency room for frequent, daily post-prandial vomiting of food occurring several hours after meals that has been developing for several months with unquantified weight loss. The in-depth questioning reveals a notion of consumption of shisha tobacco.
2.2. Clinical results
The clinical examination in average general condition did not reveal any signs of dehydration or anemia. Abdominal examination finds a fasting slap, examination of normal lymph node areas, as well as cardiovascular and pleuropulmonary examination.
3. Diagnostic Approach
On the Biological level Hyperleukocytosis without predominance on the different lineages, no inflammatory syndrome namely a normal Sedimentation Rate, CRP: negative, HIV, HBV, HCV viral serologies negative. There were no ionic disorders and no renal failure.
As part of the exploration, a morphological assessment was carried out; initially by abdominal ultrasound (Figure 1) revealing a normal liver, gallbladder, pancreas, absence of ascites, a free right iliac fossa (IMAGES A, B); furthermore, presence of a few swollen lymph nodes suggesting probable mesenteric lymphadenitis (IMAGE C).
Other investigations with a diagnostic aim were carried out, through the practice of an esogastroduodenal fibroscopy (FOGD), which revealed an irregular pylorus with an inflammatory deformed bulb, the site of a tight fibrous stenosis that could not be crossed with large ulceration (Figure 2: images A,B,C,D). Biopsies taken to look for inflammatory bowel disease (IBD), lymphoma or other pathology. The histological study concluded that the histological appearance was in favor of non-specific duodenitis and an absence of signs of malignancy.
An esogastroduodenal transit (TOGD) (Figure 3: images A, B): Bulbar serum narrowing with an inflammatory appearance suggesting, depending on the clinical context (sudden onset), a stenosis of primary peptic ulcer origin; Crohn’s disease or other cause cannot be ruled out. To support the diagnosis, an abdominal CT scan carried out showed at the post bulbar portion a filiform axial narrowing of approximately 20mm with upstream dilatation with gastric stasis (Figure 4 images A and B). To support the diagnosis, an abdominal CT scan carried out , had shown at the level of the post bulbar portion a filiform axial narrowing of approximately 20mm with upstream dilatation with gastric stasis (Figure 4 images A,B,C,D).
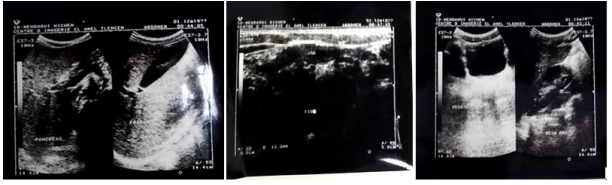
Figure 1: Abdominal ultrasound showing a gallbladder and free iliac fossa
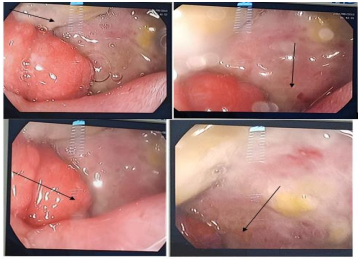
Figure 2: Esogastroduodenal fibroscopy (images A,B,C,D) showing an inflammatory bulb Site of an ulcer causing fibrous stenosis with impassable inflammatory reaction

Figure 3: Esogastroduodenal transit Images A,B showing tight bulbar stenosis
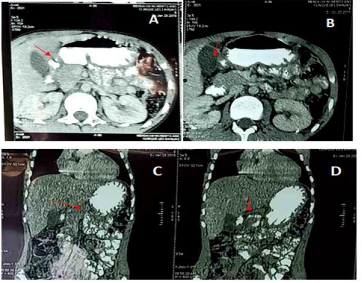
Figure 4A,B,C,D: Abdominal CT scan in sagittal section after injection of the contrast product post bulbar narrowing with an inflammatory appearance
3.1 Therapeutic Intervention and Follow-up
The child was hospitalized in the CCI department, preoperative resuscitation for a few days (6 days) was established before the surgical procedure. The approach was a midline laparotomy above the umbilical, a Mickulitz pyloroplasty was performed with transverse incision and longitudinal suture. Good postoperative outcome, the child was discharged after 10 days with referral to the consultation for monitoring and follow-up. The child was lost to follow-up until the age of 20, the patient was admitted to the medical surgical emergency room of the Tlemcen University Hospital for severe digestive bleeding with hemodynamic repercussions; a notion of taking non-steroidal anti-inflammatory drugs (Nopain cp 550 mg) for dental abscess was reported. On clinical examination, patient with extreme mucocutaneous pallor, coldness of the extremities, arterial hypotension at 80/40 mm Hg, tachycardia at 110 pul/min. Emergency blood count formula showed severe anemia at 6 gr/ dl. Given the importance of deglobulization, a blood transfusion was indicated. After stabilization of the hemodynamic constants, the patient was transferred to the gastroenterology department for further treatment. The FOGD performed revealed a reduced bulb size, deformed by large congestive folds (Figure 5 IMAGES A, B, C, D) bulbar ulcer with Forrest stage II b pigment spots.
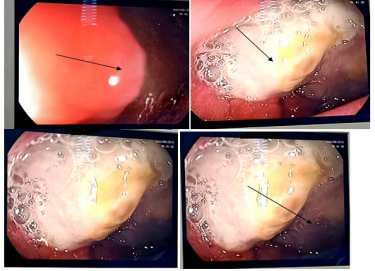
Figure 5A,B,C : Esogastroduodenal fibroscopy showing a bulb reduced in size, deformed by large congestive folds with ulcer and pigmented spots stage IIb Forrest
The endoscopic diagnosis was made, an abdominal CT angiogram was performed to look for other lesions of the digestive tract, returned normal (Figure 6 images A, B, C). Thus a treatment medical was indicated according to international recommendations by proton pump inhibitors (PPI=Inexium amp at 40 mg) at high dose intravenously (bolus 80 mg followed by a continuous infusion of 8 mg/h for 72 hours. However, persistence of melena with collapse of the hemoglobin level to 6 gr/dl justifying blood transfusions with 2 packed red blood cells and continuation of treatment by vein for 5 days. After 2 days, a very good evolution was noted, with an increase in hemoglobin to 11gr/dl and disappearance of melena. Thus was decided, relay with oral treatment including double dose PPIs with triple antibiotic therapy including amoxicillin, clarithromycin and metronidazole (14 days) and omeprazole (7 weeks) for eradication of helicobacter pylori was started. The evolution was favorable. An endoscopic check, one month later, showed complete healing of the ulcer (Figure 7). Preventive treatment of the bulbar ulcer and its complications is prescribed; the patient is currently on single-dose Lisinox PPI (cp=20mg) and dietary advice (absence of soft drinks, exclusion of spicy dishes and acidic foods).
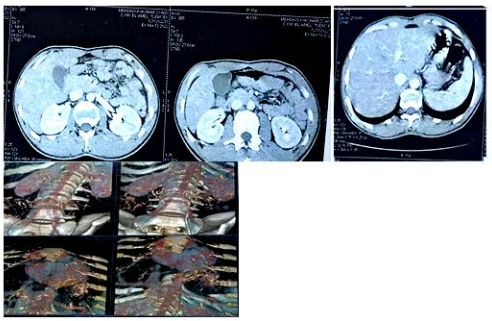
Figure 6: Thoracoabdominal CT angiogram without notable abnormalities
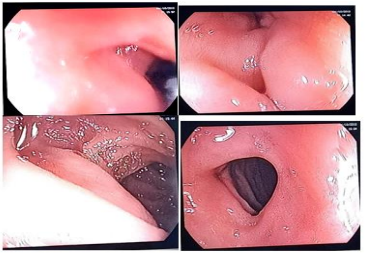
Figure 7: Esogastroduodenal fibroscopy (images A,B,C,D) healing of the bulbar ulcer
Discussion
Peptic ulcer is often diagnosed in children due to complications, the most common of which are digestive hemorrhage and perforation [2]. In our case the presentation of the ulcerative disease in the child was pyloroduodenal stenosis, which is consistent with the findings of certain authors on the rarity. The frequency of this complication in children is not documented due to a lack of studies in the literature. Duodenal ulcer mainly affects children aged over 7 years, unlike gastric ulcer which is seen earlier [3,4]. In our case, the age was 11 years old. In the literature, a male predominance is reported with a sex ratio estimated on average at 3.5 [3,5], like the case of our child. Family history is mainly observed in chronic duodenal ulcer with a percentage varying from 26 to 68% compared to 10% for gastric ulcer [4,5]. In our observation, we found no family history. The clinical expression of childhood ulcer disease depends on age and is variable. Complications can also be revealing, mainly in the form of digestive bleeding [1].
The diagnosis of post-ulcerative duodenal stenosis is evoked in the face of late post-prandial vomiting which is a constant sign accompanied by weight loss [6]. This was the revealing mode of post-ulcerative stenosis. Biology makes little contribution, the inflammatory syndrome is inconsistent, the inflammatory assessment is most often normal but does not allow another pathology to be ruled out in the acute phase [6]. Our patient’s leukocytosis is nonspecific. However, it may be absent in ulcerative duodenal stenoses. It is not a constant biological element. The blood ionogram makes it possible to assess hydroelectrolyte disorders with a view to preoperative resuscitation; in our observation we do not note any electrolyte disorders or other biological disturbances. The blood ionogram is not requested for diagnostic purposes, but to assess the impact of vomiting on the body. The usual biological picture of pyloroduodenal stenosis is metabolic alkalosis with hypokalemia and hypochloremia. Recent studies have demonstrated that these hydro-electrolyte disorders classically found in bulbar stenosis are not a common rule [7].
Abdominal ultrasound is the test that allows us to rule out a surgical emergency in the face of chronic vomiting, by showing the absence of signs of peritonitis, appendicitis or intestinal obstruction. Abdominal ultrasound is playing an increasingly important role in the diagnostic confirmation of pylorobulbar stenosis [8]. Its use dates back to 1977 [9]. This examination was carried out as first intention on the patient, and who returned normal. Esogastroduodenal fibroscopy is the paraclinical examination of choice in the diagnosis of pylorobulbar stenosis. The diagnosis is supported by abdominal CT and esophagogastroduodenal transit which demonstrate the stenosis and its topography. It is then necessary to distinguish a functional stenosis, due to the edema which accompanies an acute attack and which regresses after medical treatment, from a fixed stenosis in the context of a chronic ulcer [10]. The anatomopathological examination of the biopsy of the stenosis of ulcerative origin makes it possible to correct the diagnosis, by confirming the primary benign nature of the ulcer with the presence or absence of a Helicobacter pylori (H. pylori) infection [11]. Transit oesogastroduodenal (TOGD) currently no longer has an indication in uncomplicated ulcer disease. On the other hand, it remains of interest in the diagnosis of antropyloric stenoses [12] and nevertheless makes it possible to establish the indication for surgery. Most gastric ulcers are not visible on a CT scan because they only affect the superficial layers of the stomach wall. On the other hand, the scanner can detect them in the presence of a local inflammatory reaction or localized wall thickening [13]. The treatment of ulcer disease is mainly based on daily dietary measures and the use of PPIs. The decision on treatment is easy when the diagnosis is certain; performing an endoscopy before prescribing proton pump inhibitors is necessary. The duration of treatment is well codified. The use of a PPI is the treatment of choice providing rapid improvement of symptoms with a high cure rate. A treatment duration of 4 to 8 weeks will be necessary and a control endoscopy is warranted. The treatment surgical treatment is only reserved for complicated forms of peptic ulcer disease, dominated by ulcer perforation, hemorrhagic ulcers, pyloroduodenal stenosis, the latter was the case of our patient. Surgery is only possible after correction of hydro-electrolyte disorders and parenteral nutrition for a few days. Surgeons have the choice of operating technique. The indications depend on the patient’s ulcer history, their age and their general condition [13]. In our situation, the child benefited from a Mickulitz pyloroplasty, with good results. Postoperative consequences: It is also necessary to treat the causes of ulcers which may have been identified: stopping treatments not necessary, preferential use of paracetamol instead of anti-inflammatories such as ibuprofen, eradication of H. pylori infection [11].
The prognosis is dominated by the occurrence of ulcer recurrence and complications. The factors that are associated with a more rapid relapse are: young age, male gender, smoking, stress, the presence of H. pylori in the antral mucosa [1]. These factors are all present in our case. Ulcerative disease can be complicated at any time in its development by digestive hemorrhage (35% of cases), perforation (6 to 11%), with stenosis remaining much rarer [6]; we cannot speak healing, because the disease progresses through outbreaks, a fact reported in our observation, the child at the age of young adult presented a digestive hemorrhage. in the study by Aucouturier et al. [14] concerning UGD complicated by digestive bleeding, patients having taken NSAIDs, such as the case of our patient. The prognostic criteria are judged clinically by the importance of the hemorrhage, age, the existence of comorbidity and endoscopically according to the Forest classification [5]. Most hemorrhages of ulcer origin dry up under medical treatment (proton pump inhibitors) or when associated factors such as taking anti-inflammatory drugs are removed nonsteroidal inflammatory drugs (NSAIDs) or aspirin. Endoscopy should be performed urgently in the event of active bleeding. It makes it possible to make the diagnosis of the responsible lesion, to confirm the active nature or not of the hemorrhage and to look for endoscopic signs of recent bleeding. The description of the ulcerative lesion uses the Forrest classification [15]; the evolution under medical treatment was favorable in our patient, conrmed by the control endoscopy.
Conclusion
Duodenal ulcer disease is relatively rare in children. May be discovered at the stage of bulbar stenosis which is a complication to be considered in particular in the face of chronic vomiting. The treatment is essentially surgical. The natural history is that the ulcer disease progresses through relapse, remission and therefore can recur at any adult age in another, more serious form.
Conflict of Interest Statement
The authors declare no conflict of interest.
Author Contributions
All authors approved the final version of the manuscript.
Consent for Publication
Written informed consent to publish this information was obtained from. The parent of the study participant.
Funding Sources
None.
Declaration of Conflicting Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1. Bittencourt, P.F.S., Rocha, G.A., Penna, F.J., & Queiroz, D.M.M. (2006). Gastro-duodenal peptic ulcer and Helicobacter pylori infection in children and adolescents. J Pediatr (Rio J) 82(5), 325334.
2. Dilek O.N, Sekeer B, Dilek F.H, Oner A.F. (1995). Perforated gastric ulcer in children. Case report. Acta ChirBelg, 95(4), 182183.
3. Bott, L., Vara, D., Missotte, I., & Ménager, C. (2003). Perforation d’ulcère gastrique de l’enfant: une complication rare, à propos d’un cas. Archives de pédiatrie, 10(1), 31-33.
4. Fournier, V., Roy, P., Duclaux, I., Descos, B., & Hermier, M. (1990). Stenosing gastroduodenal ulcer in children. Apropos of 3 cases. Pediatrie, 45(4), 241-243.
5. Johnstone, J. M. S., & Rintoul, R. F. (1972). Perforated duodenal ulcer in childhood. British Journal of Surgery, 59(4), 288-289.
6. El-Nakeeb, A., Fikry, A., Abd El-Hamed, T. M., El Awady, S., Youssef, T., Sherief, D., & Farid, M. (2009). Effect of Helicobacter pylori eradication on ulcer recurrence after simple closure of perforated duodenal ulcer. International journal of surgery, 7(2), 126-129.
7. Helton, K. J., Strife, J. L., Warner, B. W., Byczkowski, T. L., & Donovan, E. F. (2004). The impact of a clinical guideline on imaging children with hypertrophic pyloric stenosis. Pediatric radiology, 34, 733-736.
8. Rosenstock, S. J., & Jørgensen, T. (1995). Prevalence and incidence of peptic ulcer disease in a Danish County--a prospective cohort study. Gut, 36(6), 819-824.
9. Starinsky, R., Klin, B., Siman-Tov, Y., & Barr, J. (2002). Does dehydration affect thickness of the pyloric muscle? An experimental study. Ultrasound in medicine & biology, 28(4), 421-423.
10. Nagura-Ikeda, M. (2020). Clinical Evaluation of SelfCollected Saliva by Quantitative Reverse TranscriptionPCR (RT-qPCR), Direct RT-qPCR, Reverse TranscriptionLoop-MediatedIsothermal Amplification, and a Rapid Antigen Test To Diagnose COVID-19 . J Clin Microbiol, 58(9), 01438-20.
11. Vergara, M., Catalan, M., Gisbert, J. P., & Calvet, X. (2005). Metaâ?analysis: role of Helicobacter pylori eradication in the prevention of peptic ulcer in NSAID users. Alimentary pharmacology & therapeutics, 21(12), 1411-1418. 1
2. Ramakrishnan, K., & Salinas, R. C. (2007). Peptic ulcer disease. American family physician, 76(7), 1005-1012.
13. Jacobs, J. M., Hill, M. C., & Steinberg, W. M. (1991). Peptic ulcer disease: CT evaluation. Radiology, 178(3), 745-748.
14. Ables, A. Z., Simon, I., & Melton, E. R. (2007). Update on Helicobacter pylori treatment. American family physician, 75(3), 351-358.
15. Nervi, G., Liatopoulou, S., Cavallaro, L. G., Gnocchi, A., Dal Bò, N., Rugge, M., ... & Di Mario, F. (2006). Does Helicobacter pylori infection eradication modify peptic ulcer prevalence? A 10 years’ endoscopical survey. World journal of gastroenterology: WJG, 12(15), 2398.
Copyright: © 2025 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



